How Multiple Myeloma Is Treated - Cancer
12-year-old Spreads Awareness On Stem Donation After Receiving Gift Of Life
Twelve-year-old Kelsey Farris is familiar with hospital visits, medical crises and pain no child should endure. Kelsey's battle with sickle cell disease began at birth. After years of searching for solutions, her doctors were able to find a cure by a stem therapy and bone marrow transplant."It's a huge blessing that she is essentially able to start life over again," said Ebony Farris, Kelsey's mother.According to NMDP, a nonprofit dedicated to cell therapy, ethnically diverse patients with blood cancers and disorders historically have had less than a 50 percent chance of finding a transplant match.Kelsey's mother and family members began testing as a match, however, health experts say 70 percent of patients do not have a match in their families. "You are more likely to match a donor who shares your ethnicity to racial background," said Erica Sevilla, a spokesperson for NMDP. "Our younger population is becoming more and more diverse, so we're going to need as possible to swab their check and join."NMDP is on a mission to diversify its donor portfolio. Officials with NMDP say African Americans, Hispanics and Asians have a more difficult time finding a match and are the ones who may require it the most.Kelsey now spends her time recovering from the transplant, creating her bucket list and spreading awareness about stem transplants."It will be hard. Very hard. But, there will be some easy things coming your way," said Kelsey. "It's important that people know out there that there are very painful and deadly disease out there and we need to do something about it, because there are a lot of people and we need to help them."Dr. Courtney Washington says the lack of donations can stem from the stigma against health care in minority communities."In the African American population, there is a big stigma on research, getting screened and tested. That is rooted in a long history in medical mistreatment of minorities. Therefore, many minorities don't get screened a lot of the times. But, it's very important we do participate and get screened because we're more likely to match someone who does have sickle cell and needs a transplant," she said.Not only was Kelsey surprised with a life-saving donor but also a visit from Grammy award winner Jon Batiste. Batiste and his wife Suleika went through similar battles trying to find a match for Suleika's cancer. "We really identified with what they went through with the bone marrow transplant process," said Ebony. "It was just amazing that he decided to become an advocate."Those interested in becoming a donor can visit here.
Twelve-year-old Kelsey Farris is familiar with hospital visits, medical crises and pain no child should endure. Kelsey's battle with sickle cell disease began at birth. After years of searching for solutions, her doctors were able to find a cure by a stem therapy and bone marrow transplant.
"It's a huge blessing that she is essentially able to start life over again," said Ebony Farris, Kelsey's mother.
According to NMDP, a nonprofit dedicated to cell therapy, ethnically diverse patients with blood cancers and disorders historically have had less than a 50 percent chance of finding a transplant match.
Kelsey's mother and family members began testing as a match, however, health experts say 70 percent of patients do not have a match in their families.
"You are more likely to match a donor who shares your ethnicity to racial background," said Erica Sevilla, a spokesperson for NMDP. "Our younger population is becoming more and more diverse, so we're going to need as possible to swab their check and join."
NMDP is on a mission to diversify its donor portfolio. Officials with NMDP say African Americans, Hispanics and Asians have a more difficult time finding a match and are the ones who may require it the most.
Kelsey now spends her time recovering from the transplant, creating her bucket list and spreading awareness about stem transplants.
"It will be hard. Very hard. But, there will be some easy things coming your way," said Kelsey. "It's important that people know out there that there are very painful and deadly disease out there and we need to do something about it, because there are a lot of people and we need to help them."
Dr. Courtney Washington says the lack of donations can stem from the stigma against health care in minority communities.
"In the African American population, there is a big stigma on research, getting screened and tested. That is rooted in a long history in medical mistreatment of minorities. Therefore, many minorities don't get screened a lot of the times. But, it's very important we do participate and get screened because we're more likely to match someone who does have sickle cell and needs a transplant," she said.
Not only was Kelsey surprised with a life-saving donor but also a visit from Grammy award winner Jon Batiste. Batiste and his wife Suleika went through similar battles trying to find a match for Suleika's cancer.
"We really identified with what they went through with the bone marrow transplant process," said Ebony. "It was just amazing that he [Jon] decided to become an advocate."
Those interested in becoming a donor can visit here.
Stem Cell Transplants Show Improved Survival Rates Across Ethnic Groups
IN a groundbreaking study, researchers have revealed significant advancements in haematopoietic cell transplants (HCT) across diverse racial and ethnic populations. While overall survival rates have improved, a stark disparity persists, particularly among African American patients.
The study, led by Nandita Khera, Mayo Clinic, Phoenix, Arizona, USA, analysed data from the Center for International Blood and Marrow Transplant Research (CIBMTR), spanning a decade and involving over 145,000 transplants. Results showed a notable increase in HCT procedures among all racial and ethnic groups, with faster growth rates observed among African American and Hispanic individuals.
HCT, encompassing both autologous and allogeneic procedures, serves as a vital treatment for various blood cancers. Despite advancements, survival rates for African American patients lag behind, with non-Hispanic African American adults and children facing 13% and 62% higher risks of death, respectively, compared to their non-Hispanic White counterparts.
Khera emphasised the need for qualitative studies to explore the impact of social determinants of health on outcomes, pointing to systemic factors contributing to these disparities. However, there is a glimmer of progress as survival outcomes for Hispanic patients now align with those of non-Hispanic White individuals.
The study underscores the importance of continued investments in research, training, and community engagement to address access and outcome discrepancies in HCT. Theresa Hahn, Roswell Park Comprehensive Cancer Center, Buffalo, New York, USA, highlighted ongoing efforts to estimate the true demand for transplants and improve accessibility.
Khera emphasised societal initiatives like the ACCESS initiative, a collaboration between the American Society of Transplantation and Cellular Therapy (ASTCT) and the National Bone Marrow Donor Program (NMDP), aimed at expanding access to HCT and enhancing outcomes for all patients. As awareness grows and collaborative efforts intensify, there is hope for a future where advancements in medical technologies benefit every individual equitably.
Reference
Khera N et al. Trends in volumes and survival after hematopoietic cell transplantation in racial/ethnic minorities. Blood Adv. 2024;DOI:10.1182/bloodadvances.2023012469.
Exploring The Frailty Factor In Stem Cell Transplant Hospitalization
In an interview with Targeted Oncology, Kayla Giannetti, MSN, APRN-CNP, discussed the background of the study, along with its findings and implications for community oncologists.
Kayla Giannetti, MSN, APRN-CNP
According to investigators, including Kayla Giannetti, MSN, APRN-CNP, frailty may be linked with extended hospital stays for patients undergoing stem cell transplants at the Cleveland Clinic. However, no other early outcomes were associated with frailty.
In the analysis, investigators sought to assess 137 adult patients that were undergoing work-up for their first allogeneic hematopoietic cell transplant between December 2021 and September 2023. "Frailty" was analyzed and defined based on specific criteria like cognitive decline, slow walking speed, or recent falls. Outcomes between "frail" and "not frail" groups were compared.
The main findings showed that frail patients were older at a median age of 64 years vs 59 years (P =.19). Frail patients also were more likely to have a Karnofsky performance status score <90 (34.4% vs 13.8%; P =.009) and had a higher intermediate disease risk index (82.5% vs 51.8%; P =.0004).
While frailty did not significantly affect whether patients could undergo the transplant, the pretransplant risk score, or the long-term survival rates, results did show frail patients to have longer average hospital stays following transplant (26 days vs 24 days), according to data presented at the 2024 Transplantation and Cellular Therapy Tandem Meetings.
In an interview with Targeted OncologyTM, Giannetti, Taussig Cancer Institute, Blood and Marrow Transplantation, Department of Hematology and Medical Oncology, Cleveland Clinic, discussed the background of the study, along with its findings and implications for community oncologists.
Multipotent stem cells in the bone marrow: © Juan Gärtner - stock.Adobe.Com
Targeted Oncology: What was the rationale behind this study?
Giannetti:We are an aging population. We also have a population that has increasing comorbidities. These factors do increase frailty and are associated with frailty. Having had a lot of treatment prior to transplant for disease also increases rates and is associated with frailty. This kind of poses the important question, does being a frail person necessarily mean that that should limit your ability to have a potentially lifesaving, curative option for your disease? That inspired me and a lot of other people to start thinking about outcomes and their association with frailty and kind of target those areas and to think about that important question deeply.
What are some of the unmet needs for this population in going through transplants?
There is a lot of work being done looking at the association with frailty and outcomes. I think it is going to be important to look even deeper into this question with another question, and that is, what kind of interventions can be done, especially early on in this process, even prior to transplant, to help decrease the rate of frailty, people who are frail becoming more frail, people who are not frail at all becoming frail at baseline going into transplant, so that they can have good outcomes. I think ultimately, that is what it is all about, having a good quality of life in addition to having this treatment option.
What were the goals of the study?
The goal of the study was to look at what association frailty has with outcomes, early outcomes, specifically. We utilized pretransplant assessment data in terms of cognitive function, physical function, as well as nutritional assessments, and looked for associations with frailty, those factors with frailty vs non-frail patients, and how that affects people without early outcomes. The early outcomes that we measured were the ability to transplant at all, the ability to be discharged, so the length of stay during your transplant admission, rate of falls during your transplant admission, if you needed [physical therapy] consult during your admission, and needing rehab after admission, so being discharged to a rehab facility, and 30-day and 100-day overall survival were the early outcomes that we looked at.
Please explain the main findings of the study.
Overall, the only significant finding that we found was length of stay for frail patients was significantly longer than non-frail patients. I do want to mention that it is going to be important to have a bigger cohort, because our sample size was on the smaller side, to really investigate those subtleties in frailty and how they are associated with outcomes.
What are the takeaways for the community or the practicing oncologist?
I would encourage the community oncologists to start thinking about these interventions early on. I think that the earlier we think about interventions, the less frail people get. It can even improve people's frailty in order to be able to potentially have this lifesaving potential curative option. Also, there is all kinds of evidence and research that is coming out that shows us what frailty looks like and there are tools being developed, like the CHARM [the Composite Health Risk Assessment Model] tool was recently developed that was presented [the 2024 American Society of Hematology Annual Meeting].
I would highly encourage community oncologists to evaluate and utilize these tools, including even with referral for transplant. There are a lot of patients who we once thought were not transplant-eligible that may be transplant-eligible. With increased referrals to transplant, we are going to have more patients being able to transplant, including older and aging population of patients.
REFERENCE: Giannetti K, Ferraro CS, Li H, et al. Impact of frailty on early outcomes post allogeneic hematopoietic cell transplant. Presented at: 2024 Transplantation & Cellular Therapy Meetings: February 21-24, 2024; San Antonio, TX. Abstract 593.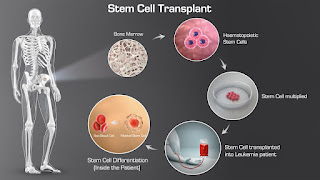



Comments
Post a Comment