New study reveals weakness in emerging type of aggressive prostate tumor - Fred Hutch News Service
A new generation of potent prostate cancer drugs has dramatically extended survival for patients with advanced prostate cancer. But prostate tumors are finding new ways of resisting these treatments, creating a need for new treatment options.
In a new study published today, researchers at Fred Hutchinson Cancer Research Center discovered that when aggressive prostate tumors turn off the receptor, their source for growth-fueling hormones, they ramp up a different growth-promoting system. When the scientists targeted this pathway in mouse models of prostate cancer, the mice lived longer.
“We figured out the mechanism by which [tumors lacking androgen receptor continue growing] … and that may be a therapeutic vulnerability,” said Hutch prostate cancer researcher and oncologist Dr. Andrew Hsieh, who led the study, which was published in the journal Science Translational Medicine. Hsieh also treats patients with prostate cancer at the University of Washington Medical Center.
In the short term, the findings could help explain why a certain class of experimental drugs has so far failed to produce results in clinical trials. In the longer term, the results could help oncologists select the right patients to treat with these drugs and pave the way for more targeted treatments.
Androgen-receptor–low prostate cancer: A growing threat
Most prostate tumors rely on the androgen receptor, or AR, which binds testosterone and related hormones, to grow and survive. Recently developed drugs, which potently block either AR or androgen production, have extended life expectancy for patients whose aggressive prostate tumors have grown resistant to other forms of treatment.
First rolled out in 2012, the drugs — which include enzalutamide and abiraterone — still aren’t a permanent cure. And when tumors recur, they find new escape routes. In 2017, Hsieh’s Hutch colleague Dr. Pete Nelson showed that after 2012, oncologists started seeing that in men whose disease had returned after treatment, significantly more tumors had rewired their molecular pathways to circumvent the need for AR. The results presented scientists with a double conundrum: First, how do the tumors continue to thrive without AR? And second, how can these tumors without AR be targeted with new treatments?
To Hsieh’s mind, answering the first question would help answer the second.
“If we can understand this process better, we might be able to find therapeutic targets,” he said.
Prostate tumors release molecular brake on growth
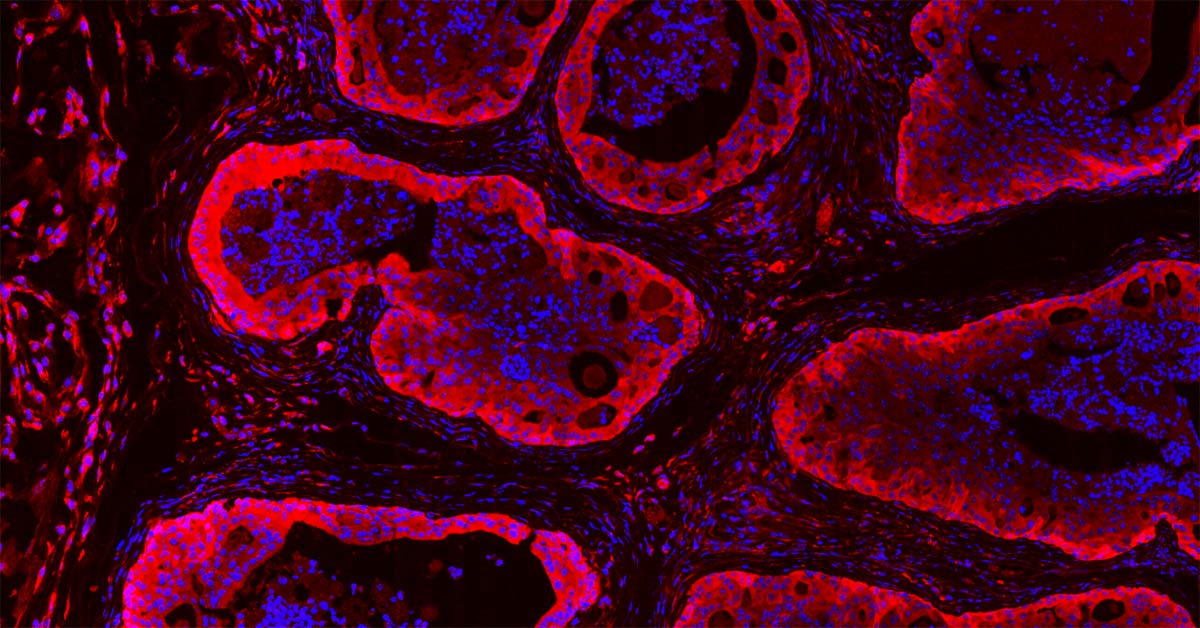
He and lab technicians Yuzhen Liu and Jessie Horn began digging to see how the new type of prostate cancer, dubbed androgen-receptor–low, or AR-low, had rewired itself. To do so, they drew on prostate cancer cells growing in lab dishes, a mouse model of the disease, patient tissue specimens, and cancer cells taken from patients with this type of tumor that are then grown in mice.
AR works by turning specific genes on. The team discovered that AR has competing effects: Sometimes it turns on genes that promote tumor growth, and sometimes it turns on genes that rein it in. When drug-resistant tumors jettison AR, they release this molecular brake and allow a growth-promoting cell-signaling pathway to compensate for others that are lost.
The molecular brake the researchers identified is known as 4EBP1. This protein works to keep production of a select group of growth-promoting proteins in low gear. By shutting off AR, tumors also shut off 4EBP1. Then, the cell’s production of these proteins shifts into overdrive. Tumor growth goes wild.
“The biggest finding at the molecular level is that the androgen receptor [in addition to turning genes on] … actually regulates protein synthesis,” Hsieh said.
https://ift.tt/2yye3o1


Comments
Post a Comment