APCCC 2019: Disparities in Prostate Cancer Management in the US - UroToday
There were 174650 new cases of prostate cancer in the US in 2019. Black Americans have approximately 2 times higher incidence of prostate cancer vs. white Americans, and ~2.5 times higher mortality.
There were 174,650 new cases of prostate cancer in the US in 2019. Black Americans have approximately 2 times higher incidence of prostate cancer vs. white Americans, and ~2.5 times higher mortality.
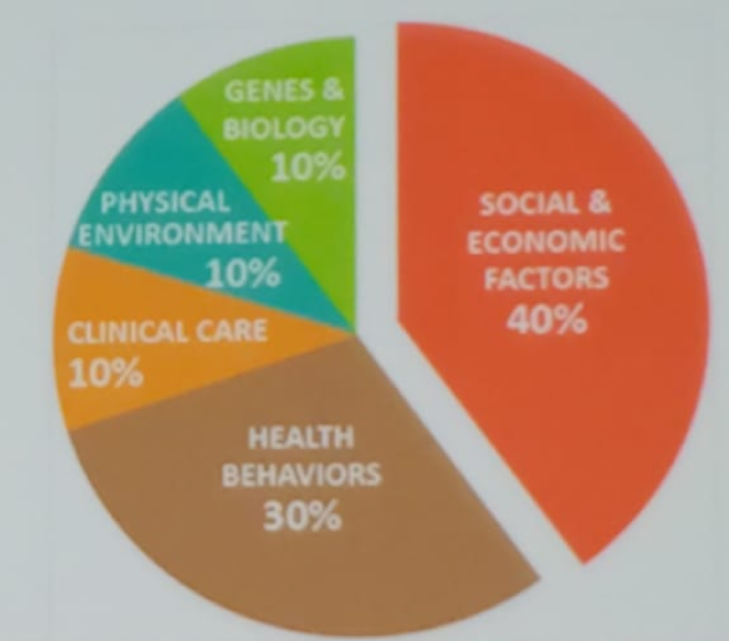
Figure 1 - Determinants of health:
An example of education and poverty driving disparity in care is the US region of the Appalachia (Figure 2). A study compared the survival between men from Appalachia to that of men, not from Appalachia from the state of Kentucky. There was considerable poorer survival in Appalachia men. This was associated with lower educational attainment, higher poverty, and greater number of comorbid illnesses.1
Figure 2 – Appalachia education and poverty driving disparity:
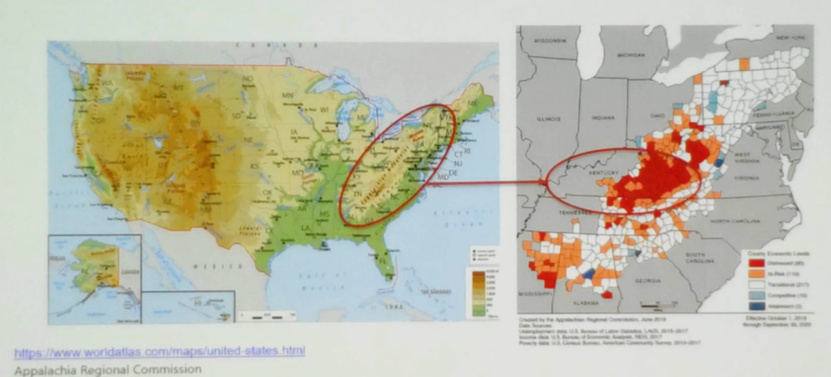
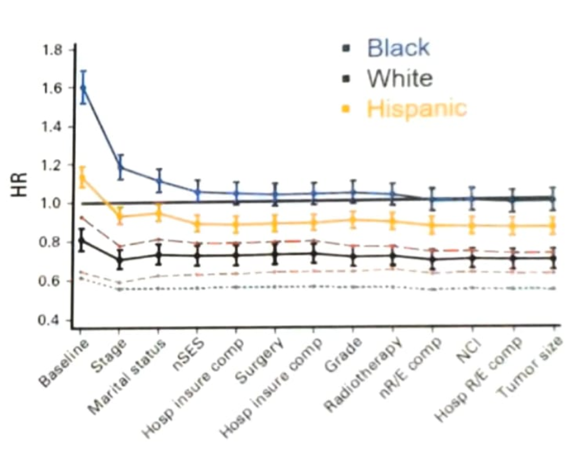
Figure 3 – Race-based disparity in California:
There have been several studies looking to assess if different disease biology confers superior outcomes. Several studies have tried to assess this (Table 1). The Abi Race study is a non-comparative pilot open-label, parallel-arm study in mCRPC patients (figure 4) attempting to help us understand if different biology confers survival benefits.
Table 1 – Studies assessing race differences: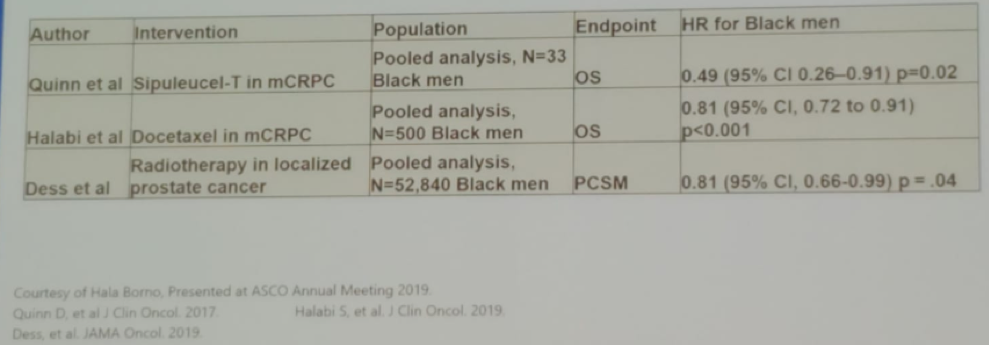 Figure 4 – Abi Race study design:
Figure 4 – Abi Race study design: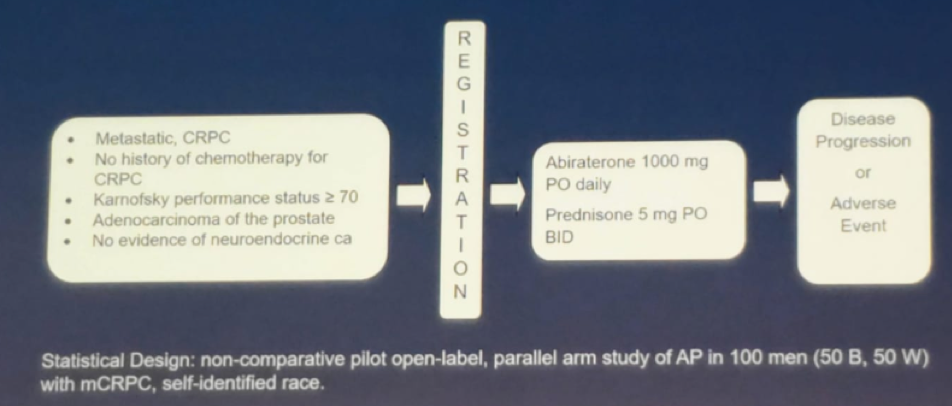 Dr. Morgans concluded her talk stating that disparities in prostate cancer in the US come in many forms, with both biological and social determinants of health contributing to this. Differences in biology may be overcome with improvements in access. Some biological improvements may be associated with improved outcomes. Efforts to enhance inclusion in clinical trials and improve access to genomic sequencing are currently underway.
Dr. Morgans concluded her talk stating that disparities in prostate cancer in the US come in many forms, with both biological and social determinants of health contributing to this. Differences in biology may be overcome with improvements in access. Some biological improvements may be associated with improved outcomes. Efforts to enhance inclusion in clinical trials and improve access to genomic sequencing are currently underway.
Presented by: Alicia Morgans, MD, MPH is an Associate Professor of Medicine in the Division of Hematology/Oncology at the Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, USA @GoldbergHanan at the 2019 Advanced Prostate Cancer Consensus Conference (APCCC) #APCCC19, Aug 29 - 31, 2019 in Basel, Switzerland
References
- Myint ZW et al. Rural and Remote Health, 2019
- Ellis L. et al. J Clin Oncol 2018
- Spratt DE et al. Jama Oncol 2016
- Spratt DE et al. J Clin Oncol 2015
https://ift.tt/2LnvNZx


Comments
Post a Comment