AUA 2020: Treating Incontinence After Prostate Cancer Surgery - UroToday
(UroToday.com) At the virtual AUA 2020 conference, nurse practitioner, Diane Newman, presented the problem of stress urinary incontinence (SUI) in men with prostate cancer (PCa) undergoing radical prostatectomy. SUI is one of the most feared complications that has been shown to be an independent predictor of global quality of life (QOL). Prevalence ranges from 2 to 90%, but decreases over time. Approximately 5–20% of men will continue to have some degree of incontinence 1–2 years after surgery. A recent prospective, a population-based cohort study of 1386 men sought to determine functional outcomes associated with PCa treatments over 5 years after treatment.4 Men undergoing prostatectomy surgery (RP) reported clinically meaningful worse incontinence through 5 years compared with all other options. Men undergoing prostatectomy for unfavorable-risk disease reported worse sexual function at 5 years compared with men who underwent external beam radiation therapy with androgen deprivation therapy.
Ms. Newman’s lecture focused on the benefits of evidence-based pelvic floor muscle (PFM) training in men with post-operative SUI. This treatment is recommended by the International Consultation on Incontinence. Assessment of SUI should precede a PFM training program. It is important to ascertain from the patient the characteristics of urine leakage, quantity (slight, moderate, severe), the number of protection pads being used (amount of saturation), when urine leakage occurs (daytime, evening when PFM fatigued, nighttime), if there is an event that triggers leakage, and if the patient voids (day or night) to determine if the bladder is able to retain urine (a sign of sphincteric support or lack of).
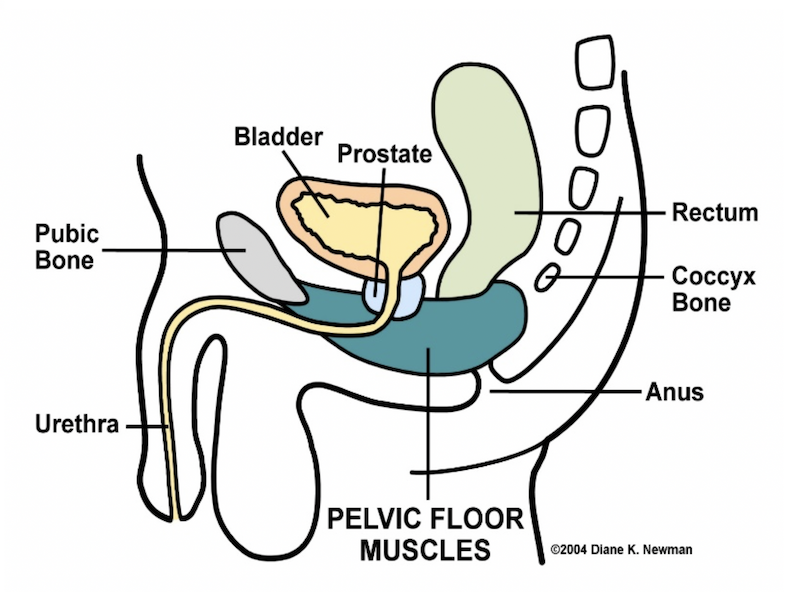
The PFMs are large skeletal muscles that sit like a hammock in the pelvic. The PFM includes 2 types of muscle fibers: Type 1 (slow-twitch muscle fibers) and Type II (fast-twitch muscle fibers). Exercising the PFMs will stimulate an increase in muscle fiber size. Hypertrophy is not an immediate training response, but strength increases are noticed long before visible hypertrophy. Exercising will increase muscle bulk. Initial assessment of the PFM in a male patient following an RP is important to determine if the muscle is: underactive, weakness present or lack of endurance of a PFM contraction or overactive, inability to relax the PFMs after a contraction, which is often but not necessarily accompanied by the presence of spasm and shortening of the pelvic floor musculature. The goal of PFM training is to improve urethral resistance and urinary control through the active exercise of the PFM. The proposed benefit of PFM training is:
- Intentional, effective PFM contraction (lifting the PFMs in an upward and forward direction) prior to and during effort or exertion clamps the urethra and increases urethral pressure preventing urethral leakage
- Bladder neck receives support from strong, toned PFM strength (resistant to stretching), limiting its downward movement during effort and exertion, thus preventing leakage.
There are 4 components to this training: 1) proper identification of muscle, 2) coordination of the PFM ability to contract and relax, 3) planned active exercise program, 4) use of muscle during an incontinent episode (the knack or stress strategy)
A PFM training program involves muscle training to improve function, tone, strength, and endurance; biofeedback to teach muscle identification and isolation for purposes of voluntary contraction and relaxation, and neuromuscular re-education or skill training to promote continence. Ms. Newman uses biofeedback (Prometheus) for PFM training as it is a method that uses a computer that records muscle activity and a monitor so the person can visualize the improvement. Biofeedback assisted pelvic floor muscle rehabilitation helps the person find the PFMs by showing changes when squeezing the right muscle, much like an athlete uses special equipment to train. Biofeedback can be used to reach a new level of strength in the PFMs. Ms. Newman described her program for PFM training in men following prostate cancer surgery. More specifics can be found here.
Presented by: Diane Newman, DNP, ANP-BC, Adjunct Professor of Urology in Surgery, Perelman School of Medicine, University of Pennsylvania and Co-Director of the Penn Center for Continence and Pelvic Health
Written by: Diane Newman, DNP, ANP-BC, Adjunct Professor of Urology in Surgery, Perelman School of Medicine, University of Pennsylvania and Co-Director of the Penn Center for Continence and Pelvic Health
References:
- Anderson et al, Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev, 2015, 1:CD001843. https ://doi.org/10.1002/14651 858.CD001 843.pub5.
- Bauer et al., Contemporary management of postprostatectomy incontinence. Eur Urol, 2011, 59(6):985–996.
- Dumoulin et al. Adult conservative management. In Abrams, Cardozo, Wein, Wagg (Eds.): Incontinence: Proceedings from the 6th International Consultation on Incontinence. Proceedings from the 6th International Consultation on Incontinence. Bristol UK: 2017:1443- 1628
- Hoffman, Penson, et al. Patient-Reported Outcomes Through 5 Years for Active Surveillance, Surgery, Brachytherapy, or External Beam Radiation With or Without Androgen Deprivation Therapy for Localized Prostate Cancer. JAMA. 2020 Jan 14;323(2):149-163.
- Newman DK Pelvic floor muscle rehabilitation using biofeedback. Urologic Nursing. 2014, 34(4): 193-202.
- Reynolds et al. Analysis of continence rates following robot-assisted radical prostatectomy strict leak-free and pad-free continence. Urology. 2010. 75(2):431–438.
- Strączyńska et al. The impact of pelvic floor muscle training on urinary incontinence in men after radical prostatectomy (RP) - A systematic review, Clin Interv Aging. 2019 Nov 12;14:1997-2005. doi: 10.2147/CIA.S228222


Comments
Post a Comment