AUA 2020: Radical Prostatectomy Versus Radiotherapy in M1a and Low Volume M1b Prostate Cancer Patients: An ... - UroToday
It is hypothesized that tumors in the early chain of progression may have a limited number of metastases because the facility for metastatic growth has not been fully reached. The CHAARTED definition of high metastatic burden was defined as four or more bone metastasis with one or more outside the vertebral bodies or pelvis, or visceral metastasis or both.
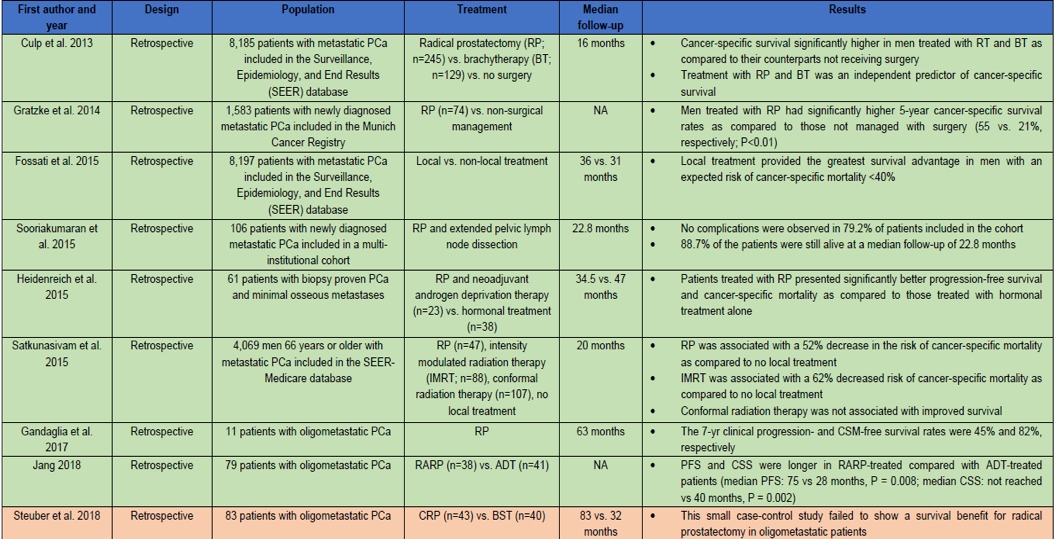
There have been several retrospective studies specifically assessing the role of radical prostatectomy in patients with metastatic prostate cancer, with variable results, as can be seen in Table 1.
Table 1 – Retrospective studies assessing the role of radical prostatectomy in patients with metastatic prostate cancer:
In the presented study, a total of 186 patients with M1a (non-regional lymph nodes, n=50) and low volume M1b (n=136) according to the CHAARTED definition (<4 bone metastases) treated with radical prostatectomy at 5 referral centers were identified. The authors assessed time to cancer-specific mortality in the entire cohort. The authors also compared the clinical recurrence rates observed in M1a patients with what was reported in the radiotherapy subgroup of the STAMPEDE arm H trial (n=92). Lastly, the authors compared the cancer-specific mortality free survival in low volume M1b patients with what was reported by the STAMPEDE trial for men who were treated with radiotherapy (n=410).
In the presented study, the median follow-up for survivors was 41 months. Overall, 90% of the patients received ADT at the time of surgery. A total of 23 patients had cancer-specific mortality. The three-year cancer-specific mortality free survival rate was 87.5%. In the M1a patients, and the 3-year complete response-free survival was similar to what was reported in the STAMPEDE trial for radiotherapy (58% vs. 51%, respectively).
M1a patients treated with radical prostatectomy demonstrated comparable cancer-specific mortality free survival rates to those treated with radiotherapy in the original STAMPEDE study (85%vs. 80%, respectively). The cancer-specific mortality free survival rates observed in patients with M1b disease was higher (84%) compared to what was reported by the STAMPEDE trial for patients treated with radiotherapy.
The authors concluded that surgery in the context of a multimodal approach, which includes ADT, might achieve comparable oncological outcomes to what was observed for patients treated with radiotherapy, who had M1a and M1b prostate cancer in the original STAMPEDE trial. These results support the potential role of radical prostatectomy in this unique setting, according to the authors. Moreover, surgery should be considered in future trials aimed at assessing the role of treatment of the primary tumor in patients with oligometastatic disease.
Presented by: Giorgio Gandaglia, Department of Urology, San Raffaele Hospital, Quinzano D Oglio Bs, Italy
Written by: Hanan Goldberg, MD, MSc., Urology Department, SUNY Upstate Medical University, Syracuse, NY, USA @GoldbergHanan at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020
References:
- Parker CC, James ND, Brawley CD, Clarke NW, Hoyle AP, Ali A, et al. Radiotherapy to the primary tumor for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. The Lancet. 2018;392(10162):2353-66.


Comments
Post a Comment