IMFINZI® (durvalumab) plus LYNPARZA® (olaparib) and IMFINZI ...
Acute Myeloid Leukemia Diagnosis
If a patients presents with the symptoms of acute myeloid leukemia a battery of tests are ordered. The tests used to diagnose AML include the following.
Blood testsFirst a complete blood count is prescribed. Anemia is commonly detected with haemoglobin levels usually less than 5g/dl. In addition there is thrombocytopenia of varying degrees. This means there is a low platelet count.
White blood cell (WBC) count is usually high but may be normal or low. The number of neutrophils is usually low.
When a small sample of blood is smeared onto a glass slide and examined under the microscope there may be presence of blast cells. This is called peripheral blood smear. The blood smear may be normal if the blast cells are confined to the bone marrow.
Blood clotting is tested by checking elevated prothrombin time, reduced fibrinogen level and the presence of fibrin degradation products. Lactic dehydrogenase levels may be raised in blood. In addition due to increased number of cell death and formation there may be raised uric acid levels.
Liver and renal function is checked especially before administering chemotherapy. In case of infections blood cultures and other appropriate tests may be prescribed.
Bone marrow biopsyIn case of an abnormal blood test, bone marrow biopsy is prescribed. The biopsy involves taking a sample of bone marrow using a syringe. The needle is pierced into the hip bone commonly and a sample is drawn. The procedure is painful and performed under a local anesthetic. The procedure takes around 15 minutes to complete and is performed on an outpatient basis.
The sample of bone marrow is checked for cancerous cells and abnormal cells. The cells are also checked to see the type of leukemia.
Lumbar puncture or spinal tapLumbar puncture involves taking a small sample of cerebrospinal fluid from the spinal column and checking for presence of abnormal cancer cells. This may be positive in patients in whom the cancer has spread to the central nervous system.
A lumbar puncture is not often used to test for AML, unless the patient has symptoms that the leukemia has affected the central nervous system. A lumbar puncture is sometimes used to deliver chemotherapy drugs into the CSF.
Cell examinationSamples of blood, bone marrow, or CSF are looked at under a microscope to check the size, shape, and other traits of the white blood cells. This helps in classifying the type of AML.
The percentage of cells in the bone marrow or blood that are blasts is particularly important. Having at least 20% blasts in the marrow or blood is generally required for a diagnosis of AML. It can also be diagnosed if the blasts have a chromosome change that can be seen in specific types of AML even if the blast percentage does not reach 20%.
Sometimes the blasts look similar to normal immature cells in the bone marrow. However, in normal bone marrow the blast count is 5% or less. In order for a patient to be considered to be in remission after treatment, the blast percentage in the bone marrow must be less than 5%.
CytochemistryThese tests include staining the leukemia cells with special dyes. For example, some of these stains cause the granules of most AML cells to appear as black spots under the microscope, but it does not cause ALL cells to change color. This helps in differentiating between the cancers.
CT scan and imaging studiesThose with AML may need to undergo imaging studies like MRI scans and CT scans to check for spread to major organs like heart, lungs, brain and liver.
Flow cytometry and immunohistochemistryThis helps in assessing the cells from the bone marrow and blood samples. These tests are helpful in determining the exact type of leukemia.
A sample of cells is treated with special antibodies that stick to the cells only if their specific protein is present on the cell surfaces. The cells are then passed in front of a laser beam. The laser light gives off light from the cells that have antibodies attached to them.
The computer can measure the number and nature of these cells. In immunohistochemistry tests blood and bone marrow samples are treated with specific antibodies so that cancer cells with proteins that bind to these antibodies change color and are visible under the microscope. These tests are used for immunophenotyping.
CytogeneticsThis involves identifying the genetic blueprints of the cancer cells. The leukemia cells atypical genetic makeup that can be identified using these tests. Identifications of the genetic abnormalities help in determining treatment.
One of the common errors or genetic mutations includes translocations. This means part of one chromosome may be replaced by part of another.
Recognizing these changes can help identify certain types of AML and predict the possible outcome of the cancer.
Common translocation include t(8;21) meaning part of chromosome 8 is now located on chromosome 21, and vice versa.
Another type of error is inversion where a segment is reversed in alignment. For example, inv(16) means that part of the chromosome 16 is upside down. Deletion, addition and duplication are other forms of errors.
Fluorescent in situ hybridization (FISH)This is similar to cytogenetic testing. This technique uses fluorescent dyes that only attach to specific parts of particular chromosomes. Once tagged to the chromosomes they are visible under a microscope in standard cytogenetic tests.
FISH can be used to look for specific changes in chromosomes. It can be used on blood or bone marrow samples.
Polymerase chain reaction (PCR)This is yet another DNA analysis test that can find some chromosome changes too small to be seen under a microscope.
Further ReadingMy Psychological Response To A Cancer Diagnosis
I believe that my brain subconsciously decided to find a shining light when I got diagnosed with a recurrence of acute myeloid leukemia (AML). Rather than the neurons going crazy over a possible death, speedy synapses in the neocortex and thalamus positioned imagination as the lead actor in the psyche cast.
"This may be an opportunity!"
If the bone marrow transplant was unsuccessful, and the end was imminent, I wondered if I would be healthy enough to have a last hurrah. I wouldn't have to worry about my meager IRAs and investments carrying me through after retirement. I had a pretty good reason to splurge.
This lucid daydream popped into my head quickly after diagnosis. I call this a confession, even though it was clearly a coping mechanism. Did anyone else do this?
I didn't tell anyone about my wandering mind; I felt that it would disturb them. But I allowed myself to scour the internet to find hidden-journey-gems in exotic locales. I had folders of different destinations that included amazing places to stay, incredible activities, first class airfare costs and more.
Was this delusional?
I want to be clear: my heart sunk when I first learned that my AML came back and that I would be getting a bone marrow transplant. The pain was at its worst when I shared the news with loved ones. Their quality of life would change too as caregivers and loving worriers.But miraculously I speedily jumped to designing an epic journey.
We all hear about the common reactions to a cancer diagnosis: anxiety, depression, sadness, anger, loss, maybe denial. But our beautiful magical brains may help us by flicking on the imagination lightbulbs. In my case, the private jet taking me to see safaris and marine excursions fed the joy receptors. I needed that.
Some may say that this distraction was a reflection of a giver-upper. But let me break it down: My preoccupied vacation-planning mind put me in a better emotional state. This welcome respite from depression taught me that I could feel positive during tough times through imagination. I liked being positive. I started to do other creative things that would make me feel positive, like writing and painting. Eventually, the desire to feel positive resulted in my will to live.
The bone marrow transplant was successful, and I was elated!
I of course realized that my outlandish trip options were irresponsible pipedreams.
Or were they?
Many tell me, "You of all people should know that life is short, and we should live out our dreams."
I stayed mostly positive during my treatment. The goal now is to continue pursuits that bring me happiness. I don't want to be a melancholy survivor. Even though I responsibly try to build my retirement fund, I also contribute to the "joy fund." These deposits are not only in dollars and cents; time spent with loved ones adds to the eminent memory bank.
For more news on cancer updates, research and education, don't forget to subscribe to CURE®'s newsletters here.
Acute Myeloid Leukemia Symptoms
The symptoms of Acute myeloid leukemia are usually slow in onset but may rapidly become severe as the number of immature white blood cells (blast cells) rises and overcrowds other cells in the blood.
The symptoms of AML are indicative of the underlying pathology of the cancer. The symptoms of AML include:-
Generalized symptomsGeneralized symptoms of AML include:
Unexplained and long term fever may be one of the symptoms. Fever is usually over 38C (100.4F). Fever is usually accompanied by excessive sweating and night sweats.
The skin and mucus membranes are pale. Mucous membranes within the mouth and the conjunctiva are usually seen to be pale. This is the hallmark sign of anemia.
Due to the rise in number of blast cells in blood the red blood cells are lowered in number and this may result in anemia. Tiredness and fatigue are symptoms that are associated with anemia and are seen commonly in AML patients. Patient may feel cold, dizzy and lightheaded.
Due to anemia many patients may also develop headaches and weakness. There may be breathlessness, palpitations and easy fatigability due to anemia and inadequate oxygenation.
LeukopeniaAs the blast cells rises in blood the adult and mature functioning white blood cells decline in number. This is called leukopenia. This causes lowering of immunity and raises the risk of repeated infections.
The patient may present with repeated episodes of infections. Some of them may be simple infections that take longer to go away and sometimes with more severe immunity-depression there may be life threatening infections.
Risk of bleedingDue to lowering of platelet counts in blood there is an increased risk of bleeding. This is called thrombocytopenia. There may be nose bleeds, heavy menstrual bleeding or bleeding from the gums.
Platelets normally help in clotting and prevent bleeding. Low platelet counts result from rising number of blast cells in blood. There may be bruises caused by minor injuries and severe and uncontrolled bleeding caused by injuries.
Bleeding may occur within the joints, in the brain etc. Creating life threatening complications. There may be bone and joint pain due to bleeding.
With thrombocytopenia and abnormal bleeding there may also be another problem of increased blood clotting or embolism or thrombosis. There may be a life threatening complication called deep venous thrombosis (DVT) or pulmonary embolism (PE) as a result.
SwellingSwollen lymph nodes are another common symptom that may be seen.
Liver and spleen may be enlarged and may be felt on palpating the abdomen.
Neurological symptomsIf the cancer affects the central nervous system there may be neurological symptoms including headaches, seizures or fits, blurring of vision, stiffness of the neck, irritability and dizziness. Some patients may experience nausea and vomiting as well.
LeukostasisThe blast cells or immature white blood cells are bigger than normal white blood cells and thus have more difficulty going through tiny blood vessels. In advanced cases, with very high blast cell counts, these cells clog up blood vessels and do not allow red blood cells to reach the peripheral organs and limbs. This is called leukostasis.
This may lead to stroke like symptoms like headache, weakness of one side of the body, confusion, dizziness, sleepiness and slurred speech. When blood vessels in the lung are affected, there may be wheezing and breathlessness.
If eye blood vessels are affected blurry vision or even loss of vision can occur. Leukostasis is rare but is a medical emergency that needs to be treated urgently.
Lumps or spots or rashesLeukemia cells especially in AML can spread to the skin. They appear as lumps or spots or rashes. A tumor-like collection of AML cells under the skin is termed chloroma or granulocytic sarcoma. AML cells may also spread to the gums causing swelling, pain, and bleeding.
Spread to other organsVery rarely AML can spread to other organs like kidneys, testes etc.
Further Reading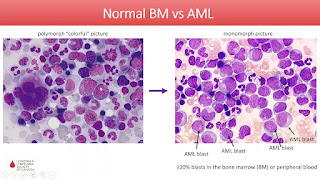


Comments
Post a Comment