Opinion | A Revolution Is Coming to Medicine. Who Will It Leave Out?
New Test For Bowel Cancer Which Can Be Done At Home Will Save Embarrassment And Pain
Procedures to check for cancers in the bowel, colon or rectum – which there are 42,000 new cases of every year – can cause discomfort so new test would help thousands
Test can eliminate need for hospital visit (Image: Channel 5)
At-home poo tests could spare tens of thousands from invasive colonoscopies to rule out cancer.
Procedures to check for cancers in the bowel, colon or rectum – which there are 42,000 new cases of every year – can cause discomfort. But new draft guidance by the National Institute for Health and Care Excellence says faecal immuno-chemical tests should be offered to patients with signs of the disease.
A sample is posted to a lab, where the amount of blood in poo is checked, with results within a week. It is hoped the move could diagnose colorectal cancer when it is more curable and cut waiting times. Bowel Cancer UK chief Genevieve Edwards said: "This will help GPs to better identify and refer the right patients for further testing quickly."
Bowel cancer checks could be done done from home (Image:
Getty Images/Science Photo Library RF)FIT tests cost between £4 and £5 and can identify about nine in 10 people with the illness. NICE found 94,291 fewer colonoscopies would take place if referrals fell by 25%, adding that NHS capacity is limited. NICE director Mark Chapman said it was "balancing the best care with value for money".
Prof Peter Johnson, NHS national clinical director for cancer, welcomed the move, saying: "GPs and hospital teams are already using FIT kits. Use tripled in the last year."
Why Britain Is So Bad At Diagnosing Cancer
Listen to this story. Enjoy more audio and podcasts on iOS or Android.Your browser does not support the <audio> element.
THE COVID-19 virus wrought havoc in Britain and killed many people. But at the start of the pandemic experts warned that unintended consequences of lockdowns might kill many more. Concerns were particularly strong with regard to cancer, as screenings were initially suspended, routine diagnostic tests deferred and the diagnosis of less obvious cases delayed. Modelling at the time suggested that disruptions would lead to thousands of additional deaths.
The grim predictions seem so far to have been correct. In cancers most picked up by early screening, death rates have returned to the levels of 20 years ago, says Nicola Barclay, a researcher at the University of Oxford. Her team's preliminary findings suggest that in colorectal cancer, the share of patients who survive for at least one year after being diagnosed has fallen from 79% just before the pandemic, to 76%. The damage cannot yet be measured for cancers that progress more slowly, or for fast-progressing diseases whose symptoms may be masked. The persistent cough characteristic of lung cancer, for example, is similar to a common symptom of covid. Deaths recorded as from covid may also blur the picture: some may have had another underlying cause of death.
The pandemic and lockdowns are not the only cause of Britain's problems in tackling cancer. Of 18 rich countries, Britain already had among the worst five-year-survival rates for three of the most common cancers: lung, colon and breast. It had more cancer deaths per person than any other G7 country (see chart). Poorer Britons are more likely both to develop and die from the disease.
It is tempting to blame Britain's woeful performance on poor treatment. But much of the gap with other countries is explained by delays in treatment, and especially by late diagnosis. "Cancer is a progressive disease, so if you diagnose cancers earlier, in almost all cases you improve cancer outcomes," says Naser Turabi of Cancer Research UK, a charity. This in part explains why the poorest, who present later, die sooner. Nine in ten people with early-stage bowel cancer, stage one, will survive for at least five years after being diagnosed. At stage four, when the cancer has metastasised, nine in ten will die.
Diagnosis usually depends on routine appointments with a general practitioner, when patients mention symptoms. Lengthening delays in patients getting to see a GP (worst again in the most deprived areas), and concerns over the overstretched NHS, well predate the pandemic. And even once referred for further tests, a target that 93% of patients with cancer symptoms should be seen by a specialist within two weeks has not been met in England for years. Another target, that patients should begin their treatment within 62 days of referral, has also been missed. That will have had deadly consequences. A study in 2020 found that every four-week delay for surgery on breast, bladder and six other tumour types increased mortality rates by 6-8%.
The government has responded to missing its targets by jettisoning them. On August 17th the NHS in England said that the existing ten cancer targets would be reduced to three. The one for a two-week wait, for example, has gone. Making the referral process more streamlined is in line with the advice of many experts, but some are still concerned. "It's a prime opportunity to bury failure," says Professor Richard Sullivan of King's College London.
There's plenty of failure to bury. In 2016 Welsh health officials travelled to Denmark to study its system. Once dubbed the cancer capital of the world, Denmark has dramatically cut cancer deaths since 2007, largely by fast-tracking cancer referrals from primary to secondary care. Although "one-stop shop" diagnostic centres, in which patients can rapidly undergo a series of tests and scans, are relatively easy to replicate, the planning that underpins them is not. For the model to work, hospital administrators must function efficiently, booking scans, appointments and treatments into a limited number of slots.
The Danish model has other advantages. Its primary-care system is better funded. Hospitals have more MRI and CT scanners per patient, and the radiologists to use them (in England the demoralised professionals are intermittently on strike). Visit Rigshospitalet in Copenhagen, the Danish capital, and cancer surgeons praise the da Vinci robots they use for complex keyhole surgery. Even more important is that specialist care is centralised, with patients bused in from rural areas to receive the highest-quality care.
Better outcomes also require recognition that 30-50% of cancers are preventable. Cancer is mostly an old person's disease, but worsening nutrition may explain an alarming rise in cases of colorectal cancer among the young. Ultra-processed food makes up more than half of a typical British diet: more than anywhere in Europe. And for all its progress, Denmark's cancer death rate is still higher than Britain's, perhaps in part because Danes smoke more.
In general there is still much to cheer in the fight against cancer. In the long run survival rates, even in Britain, have been steadily improving. Diagnoses are likely to improve further once people can conduct some tests for cancer themselves, at home, even before symptoms appear. More vaccines will be available to prevent cancers, too. That, however, is little comfort to those who were missed during the pandemic. "Once you've delayed diagnosis or delayed treatments you're in trouble," says Professor Sullivan. ■
For more expert analysis of the biggest stories in Britain, sign up to Blighty, our weekly subscriber-only newsletter.
Lee Health: Raising Awareness Of Important Cancer Screenings
Cancer detection and screening as a treatment for malignant cells with a biopsy or testing caused by carcinogens and genetics with a cancerous cell as an immunotherapy symbol as a 3D render.
Health-related observances occur on days, weeks and months throughout the year to help raise awareness of various medical conditions.
September is associated with several cancer observances, including blood, gynecologic, prostate and thyroid. Because awareness months encourage screenings for early detection, now feels like a good time to remind our community about key cancer screening tests.
Larry Antonucci
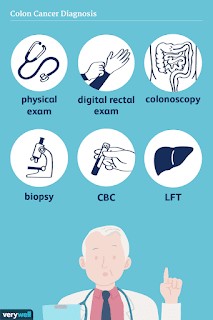
Screening tests check for cancerous cells and abnormal cells that could become cancerous, and the screenings are performed before someone exhibits any symptoms. Certain cancer screenings should be part of one's regular, proactive, preventive care because early detection often means more treatment options and better outcomes. I reached out to Mark Roh, M.D., MMM, chief physician executive for the Lee Health Cancer Institute, to review some examples of important cancer screenings. Dr. Roh and I remind you to speak to your doctor or healthcare clinician to determine the right screening tests for you based on your risk factors.
Breast cancerRegular mammograms can help detect breast cancer. Screening mammograms are recommended every year for all women starting at age 40. It is important to let your doctor know if you have a family history of breast cancer because they may want to begin mammograms before age 40.
Cervical cancerCervical cancer screening is done through a pap test performed by your primary care doctor, obstetrician-gynecologist (OB/GYN) or other healthcare clinician. For women aged 21 to 29 years old, getting a pap test every three years is recommended.
Another important screening test for cervical cancer is the HPV test, which looks for the human papillomavirus (HPV) that can cause abnormal cell changes. If a woman is 30 years old or older, she can consider pap testing every five years if it is combined with testing for HPV.
After age 65, a pap test may no longer be needed if there have been no signs of cervical precancer in the past; there has been a normal screening test for several years or if the cervix has been removed as part of a total hysterectomy for non-cancerous conditions, like fibroids.
Colorectal (colon) cancerColon cancer develops from precancerous polyps (abnormal growths) in the colon or rectum. Screening tests can find precancerous polyps, which can be removed before they become cancerous.
Screening tests can also find colorectal cancer early. The screening test for colon cancer is recommended for adults who are 45 to 75 years old.
People who are older than 75 years old should consult their doctor about screenings and whether or not they're still needed. Someone at risk for colon cancer should talk to their doctor about their options and whether they should get tested earlier than 45 years old.
Although the most known screening test is a colonoscopy, a variety of screening tests are available, and it's best to talk to your doctor about which one is right for you.
Woman Receiving Radiation Therapy Treatments for Head & Neck Cancer with Head Cast
Lung cancerYearly lung cancer screening with low-dose computed tomography (LDCT) is recommended for people 50 to 80 years old with a history of heavy smoking and who smoke now or have quit within the past 15 years. The only recommended screening test for lung cancer is a LDCT scan, where the patient lies on a table, and an X-ray machine uses a low dose of radiation to make detailed images of the lungs. The scan only takes a few minutes and is not painful. These screenings are no longer recommended after the patient turns 81 or has not smoked in 15 or more years.
Prostate cancerThe American Cancer Society recommends that men make an informed decision with their doctor or healthcare clinician about whether to be tested for prostate cancer. Starting at age 50, men should discuss the pros and cons of testing with their doctor to determine if testing is the right choice. If you are African American or have a father or brother who had prostate cancer before age 65, you should have this talk with your healthcare clinician starting at age 45. If you decide to be tested, you should get a prostate-specific antigen (PSA) blood test with or without a rectal exam. How often you are tested depends on your PSA level.
'Detecting cancer early is the key to a successful recovery'"Cancer screenings are the first step to potentially identifying serious health conditions," Dr. Roh says. "It's important not to miss them because detecting cancer early is the key to a successful recovery. If you or someone you love has tested positive for any type of cancer, know you have high-quality care and support available in your community. The Lee Health Cancer Institute is staffed with oncologists, nurse navigators, dietitians, genetics counselors, infusion services, support groups and more. Cancer treatment plans are tailored to meet each patient's specific needs."
In September, cancer services will be available closer to home for residents and visitors of South Lee and Collier counties when the Richard M. Schulze Family Foundation Cancer Clinic at the Bonita Health Center at Coconut Point opens. This new clinic will feature a 32-chair infusion center, four individual treatment rooms and 12 exam rooms. Advanced treatment options at the soon-to-open center include immunotherapy, nuclear medical scan, PET scan, MRI-guided radiation therapy, minimally invasive surgery and clinical trials.
To learn more about the Lee Health Cancer Institute, visit LeeHealth.Org/our-services/cancer-institute.
Larry Antonucci, M.D., MBA is the president & CEO of Lee Health, Southwest Florida's major destination for health care offering acute care, emergency care, rehabilitation and diagnostic services, health and wellness education, and community outreach and advocacy programs. Visit www.LeeHealth.Org to learn more.
This article originally appeared on Naples Daily News: Lee Health: Raising awareness of important cancer screenings
View comments


Comments
Post a Comment