Vinay Prasad on Cancer Screening - Econlib
MRD Testing Helped Patient With CLL Find 'Peace Of Mind'
A two-time breast cancer survivor who was diagnosed with chronic lymphocytic leukemia in 2020 discussed her belief in the power of minimal residual disease testing.
Two-time breast cancer survivor Sue D'Agostino received a diagnosis of chronic lymphocytic leukemia (CLL) in 2020, after her annual mammogram revealed enlarged lymph nodes.
D'Agostino, a 62-year-old native of Akron, Ohio, joined a support group for patients with CLL on Facebook, where she was advised to connect with a CLL specialist. That doctor discovered D'Agostino had CLL in 90% of her bone marrow, and directed her to a clinical trial, where she received three rounds of infusions of chemotherapy bendamustine and the antibody Rituxan (rituximab).
Her CLL had plummeted to 2% of her bone marrow in just three months. She moved on to the next phase of the trial, targeted treatment with Venclexta (venetoclax), along with six additional treatments of Rituxan, with a blood sample sent to the Mayo Clinic for minimal residual disease, or MRD, testing — an assessment of malignant cells remaining in the patient's body following treatment.
READ MORE: Knowing MRD Status Can 'Increase Chance of Cure' in Blood Cancer
"My first one came back and (it) was April of '21, and they said I was MRD negative," D'Agostino said. "So, they test one in 10,000 and 100,000 cells and I was in complete remission in my blood." A September 2021 biopsy found that she was also in remission in her bone marrow.
D'Agostino, who still has her bloodwork checked every three months, spoke with CURE® about her belief in MRD testing.
Transcript:
I don't know if it's just a cost thing that a lot of people don't do it, but I would definitely encourage everybody to get an MRD test. Here again, I don't know what the cost is and I don't have insurance (that covers it) — because this was a clinical trial, it was all part of it. But just for me, it was (about) peace of mind, because it's a nagging thing. Especially for me, when I found out that CLL was in 90% of my bone marrow, that's a lot, and then to tell me, it's gone it, there's no CLL on your bone marrow. It's quite a relief. And I encourage everybody that's in my group (to) talk to your doctor about this, you know, see where you're at, because they'll tell you.
I have a girlfriend that got to 20(%), she was she was at 70(%), she did a clinical trial. And she got to 21%. So, she didn't make it to two MRD. But now she knows that. And so, she's already started another treatment, because you just want to try and knock that down and keep it at bay, if you're not going to be in remission. So that would help you to know, because there are a lot of targeted treatments out there like venetoclax, and you take those, if you can't get it down to MRD negative, you take those basically until they don't work. That could be five years, it could be 10 years, it could be whatever. And then there are so many new treatments and new clinical trials out there that by the time maybe that one stops working, you know, you move on to your next one. And you know, who knows that month that one might be the one to get you to MRD negative.
This transcript has been edited for length and clarity.
For more news on cancer updates, research and education, don't forget to subscribe to CURE®'s newsletters here.
Chronic Lymphocytic Leukemia: Slow-Appearing Symptoms
New therapies are transforming treatment
Halfpoint Images / Getty Images
Medically reviewed by Gagandeep Brar, MD
Chronic lymphocytic leukemia (CLL) is a bone marrow cancer leading to abnormal white blood cells in the blood. It's slow-growing and mainly affects older adults. It can be years before chronic lymphocytic leukemia needs treatment, and treatments can keep the worst symptoms at bay for many years.
In this case, "chronic" means the cancerous cells are partially mature. The cancer cells look normal but don't work as well and live longer than healthy cells. This cancer takes time to show symptoms.
Halfpoint Images / Getty Images
CLL is slow growing but very hard to cure. As the disease progresses, the defective cells grow and spread to the lymph nodes, liver, and spleen. A bone marrow transplant is the only cure but is not often the best treatment choice. Many people live with this cancer until they die of other causes.
This article will explain chronic lymphocytic leukemia, the symptoms and treatments, and what people can expect regarding life expectancy, survival, remission, and relapse rates. It will also advise on living with this slow-growing cancer with lifestyle, medical treatments, and ways to improve quality of life.
Acute vs. Chronic Lymphocytic LeukemiaChronic lymphocytic leukemia is just one of many types of leukemias (cancers of the white blood cells). Specifically, CLL differs from acute lymphoblastic leukemia because of how mature the cancer cells are.
Leukemia TypesLeukemias are classified as myeloid or lymphocytic depending on what precursor cells the cancer starts in. Lymphocytic, lymphoid, or lymphoblastic leukemias start in the cells that become lymphocyte white blood cells. Myeloid leukemias begin in the bone marrow cells that become other types of white blood cells, red blood cells, and platelets.
Chronic leukemia cells mature partly and look more like normal white blood cells than other leukemia cells. Acute leukemias have cancer cells that look more immature, wild, and defective. Chronic leukemias are slow growing but are more complicated to cure than acute leukemias.
CLL often affects older adults. It's rare in children but is the most common leukemia in adults—accounting for about 38% of new leukemia cases in adults. Estimates for 2023 suggest 18,740 new cases and 4,490 deaths from CLL. It is more common in men than women. The terms for sex or gender from the cited source are used.
Related: Major Differences Between Leukemia and Lymphoma
Symptoms: Do I Have Chronic Lymphocytic Leukemia?Most of the time, people diagnosed with chronic lymphocytic leukemia do not have symptoms. It's often found based on blood tests done for other reasons.
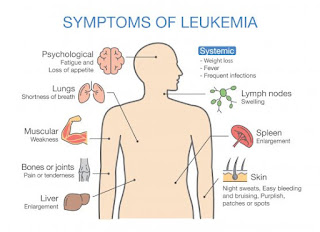
The symptoms of chronic lymphocytic leukemia often are vague and are also symptoms of diseases other than cancer. Chronic lymphocytic leukemia symptoms include:
If you have these symptoms, abnormal blood tests, and are the right age for chronic lymphocytic leukemia, your healthcare provider will order tests to diagnose chronic lymphocytic leukemia.
Tests include:
Complete blood count (CBC) test to measure many types of cells in your blood: Too many lymphocytes are a sign of chronic lymphocytic leukemia.
Test of the cells in the bone marrow: A healthcare provider samples the tissue with a needle, and a pathologist checks it for leukemia cells.
The pathologist may also check other blood, bone marrow, and lymph node samples to determine the kind of leukemia.
Blood tests will check your liver, kidney, and other organ function.
Imaging tests, usually computed tomography (CT) scans, check for cancer in your lymph nodes, spleen, or liver.
Most cases of chronic lymphocytic leukemia do not have a cause. Risk factors include older age, exposure to chemicals (research has linked exposure to Agent Orange herbicide, other pesticides, and radon to chronic lymphocytic leukemia), family history of leukemias, and sex.
Secondary Chronic Lymphocytic Leukemia ComplicationsBone marrow in CLL makes new, abnormal lymphocytic white blood cells faster than usual. They live longer than they should and crowd out normal cells. As the body's abnormal white blood cells build up, so do the signs and symptoms of advanced CLL.
Red blood cell and platelet counts drop, and normal white blood cells die off. This can cause several complications, including:
Anemia: A lack of red blood cells causes tiredness, weakness, and shortness of breath.
Leukopenia: A lack of normal white blood cells increases infection risk.
Neutropenia: A lack of healthy neutrophils (a type of white blood cell that usually is most numerous in the blood) increases infection risk.
Thrombocytopenia: A lack of platelets causes excessive bruising and bleeding (including severe nosebleeds and bleeding gums).
Many of these complications put people with CLL at a higher risk of infection. This might mean frequent colds, cold sore outbreaks, or a higher risk of developing illnesses like pneumonia (lung infection) or fungal infections.
The cancerous white blood cells in CLL may also make abnormal antibodies that attack normal blood cells—a complication known as autoimmunity. It may also cause autoimmune hemolytic anemia, in which the antibodies attack and destroy red blood cells.
As chronic lymphocytic leukemia advances, it can transform into more aggressive cancers that may be harder to treat, including:
Acute myeloid leukemia may develop due to treatment that damages myeloid white blood cell precursors rather than CLL transforming into it.
How Successful Is Chronic Lymphocytic Leukemia Treatment?Many people with CLL do not die of it. Only about one-third need treatment. Many are older (the average age at diagnosis is 70), and often, because the cancer is slow-growing, they may die from other causes before needing treatment. In one-third to one-half of cases, infections may kill the person before the cancer does.
If chronic lymphocytic leukemia advances and needs treatment, it can be tough to cure. But as new therapies are developed, many people can live years without their disease worsening.
Staging and Risk GroupsHealthcare providers determine the best treatment options and prognosis for people with chronic lymphocytic leukemia based on the stage of their disease. Staging is a way of comparing cancers, treatments, and predictions and is determined during diagnosis.
There are two different staging systems used for chronic lymphocytic leukemia. Doctors in the United States use the Rai system based on the number of lymphocytes in their blood and bone marrow.
The following stages are used for chronic lymphocytic leukemia:
In stage 0, the blood has too many lymphocytes in the blood, but there are no other signs or symptoms.
In stage 1, the excess of lymphocytes makes the lymph nodes more significant than usual.
In stage 2, the abnormal lymphocytes in the blood make the liver or spleen larger than usual.
In stage 3, there are too few red blood cells. The abnormal white cells have made the lymph nodes, liver, or spleen larger than usual.
In stage 4, the blood has too few platelets; the lymph nodes, liver, or spleen, are more significant than usual, or there are too few red blood cells.
Doctors separate the five Rai stages into low-, intermediate-, and high-risk groups.
The Binet staging system is more common in Europe. It classifies chronic lymphocytic leukemia by the lymphoid tissue groups affected. This includes the neck lymph nodes, groin lymph nodes, underarm lymph nodes, spleen, and liver. It also takes into account anemia and thrombocytopenia. The stages are A, B, and C, by how advanced the disease is.
Other Factors in PrognosisOther factors play a role in a person's prognosis. Factors that negatively impact prognosis include:
Older age
Worse overall health
Genetic changes, including deletions on chromosomes 17 or 11 or duplication of chromosome 12
High levels of the proteins ZAP-70 and CD38 in the cancer cells
Cancer that has spread to the spleen, liver, or lymph nodes
The presence of symptoms
Cancer that has come back or has not responded to treatment
A higher volume of bone marrow has been replaced by cancer cells
High blood levels of beta-2-microglobulin
A lymphocyte count that doubles in less than one year
Higher levels of immature lymphocytes in the blood
An unchanged immunoglobulin heavy chain variable region (IGHV) on the cancer cells
Missing TP53 gene on the cancer cells
As chronic lymphocytic leukemia progresses, it has four stages, as follows:
Asymptomatic, in which cancer causes no or few symptoms
Symptomatic or progressive, as cancer causes severe symptoms
Recurrent cancer that has come back after a period of remission
Refractory cancer does not get better with treatment
People with slow-growing low-risk CLL will not need treatment right away. Research has shown that treating this cancer early does not help people live longer. In the asymptomatic phase, healthcare providers will often wait on treatment and monitor the blood counts until the disease worsens or you start having bothersome symptoms.
Because people with chronic lymphocytic leukemia are usually older and CLL progresses slowly, one-third of people diagnosed with it will never need treatment.
About 88% of people over age 20 diagnosed with chronic lymphocytic leukemia are alive five years later. That doesn't tell us much since many people with CLL will live years and years without even needing treatment.
Veterans With CLLBecause of the potential link between Agent Orange and leukemias, veterans with chronic lymphocytic leukemia exposed to Agent Orange or other herbicides during military service are eligible to receive health care and disability compensation from the Department of Veterans Affairs.
After Diagnosis: Chronic Lymphocytic Leukemia Treatment PlanMost people will wait on treatment until they have symptoms. When they need treatment, the first-line therapy for chronic lymphocytic leukemia has long been chemotherapy-immunotherapy. However, new targeted therapies have been developed. You may also need surgeries (like spleen removal) or radiation to reduce symptoms.
For many, treatment can prolong disease-free survival for many more years, even after they have symptoms and need treatment. New, targeted therapies called Bruton tyrosine kinase inhibitors significantly affect survival and quality of life.
Healthcare providers test new drugs and new drug combinations in clinical trials. Clinical trials should be a treatment option for anyone with chronic lymphocytic leukemia.
Researchers are still studying the impact of these targeted therapies on survival, but their impact seems significant. They can be used until they stop working, unlike chemotherapy, which is too toxic to be used for long periods. Studies have shown that:
After four years on Calquence (acalabrutinib), 88% of people were still alive.
After two years on Brukinsa (zanubrutinib), 94% of people were still alive.
After seven years on Imbruvica (ibrutinib), 78% of people were still alive.
In addition to new treatment options, there is a significant difference in survival based on the type and stage of chronic lymphocytic leukemia. CLL is classified into these two types:
The slow-growing type which low levels of ZAP-70 and CD38. People with this type may live for five to 10 years or longer.
The other kind has high levels of ZAP-70 and CD38, grows faster, and is a more severe disease. Those with very high-risk types may be referred for a stem cell transplant early in treatment, which can potentially cure the disease.
For many, chronic lymphocytic leukemia treatment can be so effective that there are no signs of leukemia—known as complete remission. Though there is no cure, most people with CLL can undergo long periods of successful treatment without getting sicker.
But this disease often comes back at some point, so even if you're in remission, it will not likely be a cure. Most people will relapse within the first five years of starting treatment. After first-line treatment with chemotherapy, 6% of cancers will return within 12 months, and another 14% will do so within two years.
Targeted therapies are more effective at prolonging progression-free survival than chemotherapy. Researchers are still studying the remission rates for these newer targeted therapies. How many people eventually relapse and require a new type of treatment is still unknown.
Self-Care With Chronic Lymphocytic LeukemiaMost people live with CLL for many years. About one-third will live out their lives and die from other causes without needing treatment. The rest will need treatment eventually, sometimes for years. Treatment, especially with chemotherapy, may stop for a while, but it never really ends.
Taking care of yourself during this time is essential. Living with cancer that will not likely be cured can be difficult and stressful. Remember that your healthcare team is there to help, and you can do your part by taking care of your body, such as in the following ways:
Your treatments may cause side effects: Tell your care team—they may be able to lower the dose or switch your treatment.
You may feel exhausted from your disease: Eat well and be active when you can. If you have anemia, your healthcare provider may recommend a transfusion.
Related: What to Eat When You Have Chronic Lymphocytic Leukemia?
Support for Advanced Chronic Lymphocytic LeukemiaMany people with cancer feel depressed, anxious, or worried. Though chronic lymphocytic leukemia can take a long time to progress, it can be hard to live with the threat of cancer returning or getting worse hanging over your head.
You can benefit from leaning on friends, family, and community and finding support groups, professional counselors, or others to help you cope on your cancer journey.
Know that many new drugs have been developed for this disease; ask your healthcare provider about clinical trials. New therapies for CLL are helping people, even those with advanced disease, live longer, often with a higher quality of life than other treatments.
Many people with chronic lymphocytic leukemia stay on these treatments—sometimes without their disease worsening—until they die of other causes.
Studies have shown that about one-third to one-half of people with chronic lymphocytic leukemia die from infections. Your healthcare provider can take steps to help you fight off infections. These may include vaccines, medicines like antivirals, or other treatments.
Other people with chronic lymphocytic leukemia die from the effects of the cancer cells on different parts of the body, which stop these organs from functioning normally.
Advanced chronic lymphocytic leukemia is hard to cope with when drugs are no longer working. You'll need to decide which treatments are suitable for you.
Palliative care aims at reducing symptoms of cancer and its treatment and helping you reach your goals—whether that's staying active or staying at home.
SummaryChronic lymphocytic leukemia is a type of blood cancer. It affects the bone marrow and causes an increase in abnormal lymphocytic white blood cells. It is most common in adults around age 70 and progresses slowly.
In CLL, the cancer cells occupy space and crowd out healthy cells. Symptoms of CLL can take a long time to appear. It's often discovered during tests for other reasons. Healthcare providers use blood, bone marrow, and imaging tests to diagnose CLL.
Chemotherapy and immunotherapy used to be the treatment of choice for CLL. Now, targeted therapies are usually the best option.
Not all people need treatment immediately, especially if their CLL grows slowly and is low risk. Starting treatment early doesn't always improve survival rates. Instead, healthcare providers suggest watchful waiting, which is when your provider monitors you before starting treatment.
How long someone with CLL will live depends on their age, health, genetics of their cancer, and the cancer's stage. Many people with CLL don't die from the disease itself.
Living with CLL involves managing symptoms and treatment side effects and improving quality of life. Complications include anemia, a higher risk of infections, and abnormal antibodies. Regular checkups and maintaining a healthy lifestyle are essential.
View comments
Leukemia And Oral Symptoms: Swollen Gums, Bleeding, And More
Leukemia is a type of cancer that affects blood cells. It begins when a cell's DNA in the bone marrow or other blood-forming tissues mutates, causing blood cells to develop and function abnormally. These abnormal blood cells are leukemia cells.
Leukemia is a systemic disease, meaning that it affects blood components throughout the entire body. Leukemia may cause a hematoma — pooling of the blood under the skin — and bleeding in various areas of the body, including the mouth.
It's easy to overlook minor symptoms like swollen or bleeding gums, but they may be one of the earliest signs of some types of leukemia.
"We see our patients more frequently than the primary care physician, and often a dentist may be the first doctor that notices the symptoms of leukemia," says Jessica Pharar, DMD, the founder of the Pharar Foundation, an organization in Las Vegas that provides specialized dental care for patients with cancer and other chronic conditions.
Leukemia cells may also infiltrate the gums, causing unusual gum lesions or inflammation, which your dentist may notice.
"We will usually reevaluate a concerning area [such as inflamed gums] in two weeks to allow your body to heal the area. If the concerning lesion does not heal within two weeks, we will then progress the care to another provider, such as an oncologist," Dr. Pharar explains.
According to an article published in Hematology, Transfusion and Cell Therapy in 2022, oral symptoms were most commonly seen in the following types of leukemia:
Not everyone with leukemia experiences oral symptoms, according to Sudarsan Kollimuttathuillam, MD, a medical oncologist and hematologist at City of Hope in Huntington Beach, California. "However, it is fairly common during treatment of leukemia, especially chemotherapy," he says. "[Leukemia] and its treatment can affect the mouth in various ways such as bleeding gums, overgrowth of the gums (gingival hyperplasia), ulcers, and inflammation of the mouth."
Other oral symptoms seen in leukemia are:
When these signs and symptoms do exist, they are usually a result of:
Blood clotting problems Leukemia can affect the level of platelets in your body, which are the cells that help your blood clot. Disruption of your body's natural clotting processes may cause easy bleeding or bruising of the gums, tongue, or lips.
Treatment effects Sometimes leukemia treatment causes side effects that affect the teeth, mouth, and jaw. For example, chemotherapy can cause dental issues such as mouth sores, tooth decay, pain, and dry mouth.
Infections People with leukemia are at higher risk for infections like oral herpes and candidiasis because of a weakened immune system. These infections can cause symptoms like sores, blisters, and white lesions on the mouth.
RELATED: What Are Common Symptoms of Leukemia?
Tips for Reducing Mouth Pain and Other SymptomsLeukemia's effect on the mouth may cause other problems that can significantly reduce your quality of life.
Try the following strategies to soothe and reduce your mouth symptoms.
Some oral symptoms will improve on their own, while others will need treatment. For instance, gum issues may improve or resolve as the cancer goes into remission. But "damage to the teeth and salivary glands due to leukemia treatment would require additional, separate dental treatment," Pharar says.
If you have already received a diagnosis of leukemia, consider prioritizing your dental health as part of a holistic treatment approach. It is best to work with your healthcare team, including your dentist, to ensure optimal dental health during and after your treatment.


Comments
Post a Comment