APCCC 2019: De Novo Oligometastatic Prostate Cancer: Consensus and Controversy on Aims, Options and Rationale - UroToday
We currently have level 1 evidence that AR-directed therapy improves OS in M1 disease, provided by mutually supportive, well-conducted phase III randomized prospective trials:
- STAMPEDE1: M0 or M1 patients treated with ADT vs ADT + abiraterone acetate and prednisone (HR 0.63, 95% CI 0.52-0.76)
- LATITUDE2: M1, high risk patients treated with ADT vs ADT + abiraterone acetate and prednisone (HR 0.62, 95% CI 0.51-0.76)
- ENZAMET3: M1 patients (all comers) treated with ADT vs ADT + enzalutamide (HR 0.67, 95% CI 0.52-0.86)
- TITAN4: M1 patients (all comers) treated with ADT vs ADT + apalutamide (HR 0.67, 95% CI 0.51-0.89).
According to Dr. Morris, the primary may be an active participant in tumor self-seeding as well as generating metastatic disease. Whole genome sequencing has shown cross-pollination of metastatic disease in mCRPC in that metastatic lesions were often more similar to each other than the primary. Furthermore, similar metastatic lesions were often in geographic proximity, a phenomenon known as interclonal cooperativity5.
The STAMPEDE arm H radiation therapy to the primary lesion6 was built on the HORRAD data, randomizing patients to standard of care +/- radiation therapy to the primary. Importantly, the study was powered to assess low volume disease independent of the larger treatment group. This study found that among 819 low volume patients, radiation therapy to the primary improved OS (HR 0.68, 95% CI 0.52-0.90). Confirmatory studies of this finding are currently underway and include PEACE-1, SWOG 1802, TRoMbone, and G-RAMPP.
Small studies have assessed metastasis directed therapy vs no therapy, including a Japanese study of 40 patients with bone metastasis and node positive prostate cancer7. Among these patients, 18 received metastasis-directed radiation therapy to all metastatic sites. Oligometastatic disease was defined as the presence of five or fewer metastatic lesions. Over a median follow-up of 62.5 months among all patients, the 5-year castration-resistant prostate cancer (CRPC)-free survival rate and cancer-specific survival was 64.4% and 87.9%, respectively. Patients treated with metastasis-directed radiation therapy had a significantly higher probability of achieving a PSA level of <0.02 ng/mL than those without the therapy (88.8% vs 54.5%, p = 0.035) and consequently had a better CRPC-free survival than those without the therapy (HR 0.32, 95%CI 0.12-0.88).
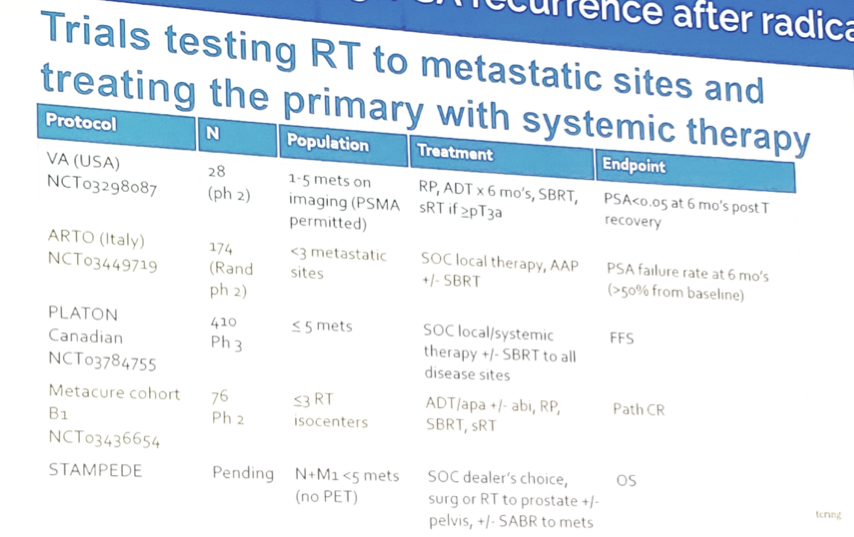
Currently, there are ongoing trials of radiation therapy to metastatic sites and treating the primary with systemic therapy, including STAMPEDE arm M:
Dr. Morris concluded his presentation with several summary points:
- There is a subset of M1 patients with the primary still in place
- There is no justification for denying these patients systemic therapy – we have level 1 data, which has been confirmed many times over. However, the duration of therapy remains an open question
- The rationale and data support radiation therapy to the primary lesion, and confirmatory studies are needed and underway
- Radiation to the metastatic lesions are anecdotal and not standard of care, as there is currently no prospective data. Furthermore, we need real endpoints that we can interpret
Presented by: Michael J. Morris, MD, Memorial Sloan Kettering Cancer Center, New York, New York
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md at the 2019 Advanced Prostate Cancer Consensus Conference (APCCC) #APCCC19, Aug 29 - 31, 2019 in Basel, Switzerland
https://ift.tt/2LmSnBg


Comments
Post a Comment