AUA 2020: Androgen Deprivation Therapy (ADT): Reducing Morbidity and Improving Outcome - UroToday
(UroToday.com) Dr. Laurence Klotz gave a presentation elaborating on how to reduce the morbidity and improve the outcomes of androgen deprivation therapy (ADT).
The objectives of this talk were to understand the long-term effects of ADT and its association with cardiac disease, metabolic syndrome, bone health, cognitive function, and quality of life. Dr. Klotz also planned to review the importance of serum testosterone levels in men receiving ADT. Additional goals of this talk included a comparison of intermittent versus continuous ADT use in prostate cancer patients, and discussing the role of ADT in the androgen receptor antagonist therapy (ARAT) era.
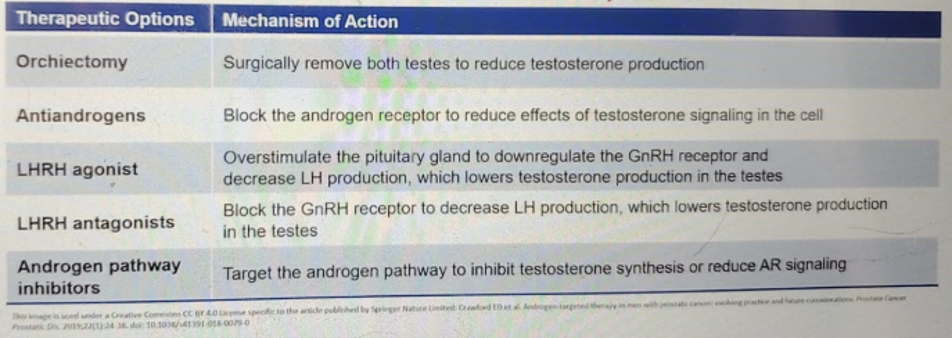
Dr. Klotz began with a detailed outline of ADT adverse effects. The mechanism of action of ADT is summarized in Table 1, outlining the various options of ADT.
Table 1 – ADT options and mechanisms:
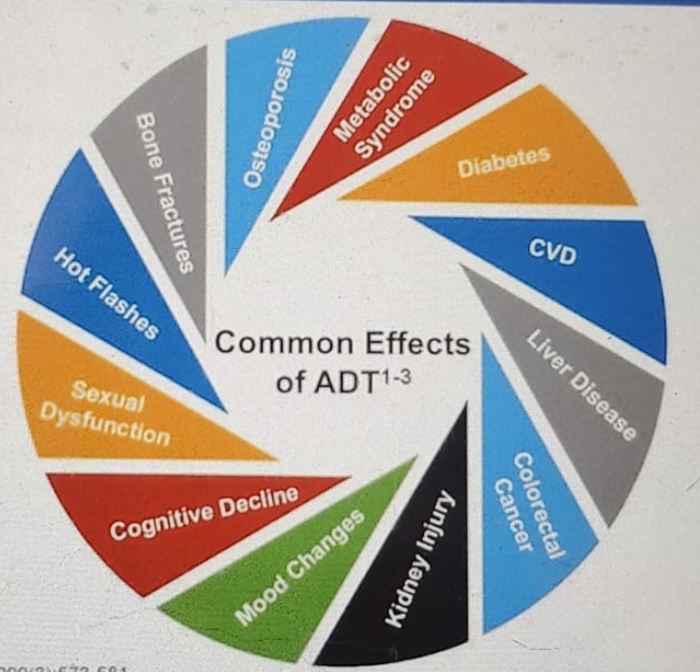
ADT has a multitude of adverse effects, impacting all systems of our body from cardiovascular, bone health, sexual dysfunction, hepatic disease, and cognitive function (Figure 1).
Figure 1 – ADT adverse effects:
The adverse effects were discussed in detail in the next part of Dr. Klotz's presentation:
- Hot flashes are one of the most common short-term effects of androgen deprivation therapy. They are defined by sudden diaphoresis and facial discomfort. It is usually the most common complaint, affecting up to 80% of men treated with ADT. Management recommendations include lifestyle modifications, which consist of avoidance of known triggers, and implementation of relaxation techniques. There are various medications that can be given, including hormonal and non-hormonal drugs, and acupuncture has been shown to help as well.
- Sexual dysfunction affects over 90% of men treated with ADT. Loss of libido is manifested by 58 to 91% of men, and erectile dysfunction occurs in 73 to 95% of men. Managing recommendations for this problem include counseling and referral to psychosocial and or sexual rehabilitation experts. Medications, including PDE 5 inhibitors, can be tried, and intracavernosal injections can be administered. Other options include devices and penile prosthetics. It is important to remember that intermittent androgen deprivation therapy enables androgen recovery between treatment cycles and that men receiving this type of treatment have been shown to have greater sexual desire and sexual activity compared to men who receive treatment on a continuous basis.
- Cognitive impairment in men being treated with ADT has been studied as well. Retrospective cohorts have shown an increased risk of cognitive impairment in men using ADT. However, in prospective cohorts, no such association was demonstrated.
- ADT has also been shown to increase the risk of dementia by 20% and Alzheimer's disease by 14%.
- Psychological effects are also seen more commonly in men being treated with ADT. It has been shown that ADT increases the risk of significant distress by 33%. Moreover, a 23% increase in depression rates has been noted in men using ADT, and it also raises the risk of suicide by 4-fold. The management recommendations include referral to a psychiatrist or psychologist if deemed appropriate. Other recommendations include psychosocial interventions, including education packages and patient support. Additional alternatives include antidepressants prescription.
- ADT is also associated with a decrease in bone mineral density as well as an increased risk of fracture. ADT raises the risk of bone fractures by 39%, and it raises the risk of osteoporosis by 49% after four years of treatment, and by 80% after 10 years of treatment. Men being treated with ADT demonstrate a decline in bone mineral density and in total body mass. The fracture rate is positively associated with the cumulative ADT dose. Recommendations for the management of decreased bone mass density are extremely important. These include performing a baseline DEXA scan for bone density assessment and repeat it every one to two years under treatment. Patients should be engaged in regular aerobic and weight-bearing exercise. Alcohol and smoking should be stopped, and pre-treatment dental assessment should be made to reduce the risk of osteonecrosis of the jaw.
Active treatment includes bisphosphonates, alendronate, or zoledronic acid. Patients should also be encouraged to take daily calcium and vitamin D supplements.
- Metabolic syndrome is also a significant risk factor for men with ADT. They have a 25% increased risk of developing metabolic syndrome, and a 28-44% increase risk of developing diabetes. The prevalence of diabetes in men with ADT is significantly higher than that in men without ADT (52-55% vs. 22-36%). Metabolic syndrome diagnosis is mainly driven by abdominal obesity, hyperglycemia, and elevated triglycerides.
- Sarcopenia is also associated with ADT use. There is a 22% increased risk in gaining visceral abdominal fat after 12 months with ADT. Approximately 70% of men receiving ADT will develop sarcopenic obesity.
Startin use in these patients with metastatic prostate cancer may delay the progression of castrate-resistant prostate cancer. Statins have been shown to improve castrate-resistant prostate cancer-free survival and cancer-specific survival.
Another potential beneficial medication is metformin, which has been assessed quite extensively with its effect on prostate cancer patients. Metformin has been shown to generally reduce the incidence and mortality of cancers. It increases the response to treatment in cancer cells when using radiotherapy and chemotherapy, and it optimizes tumor movement and reduces the malignancy. It also reduces the likelihood of relapse and decreases the damaging effects of ADT.
Metabolic syndrome and diabetes should be regularly monitored and treated in prostate cancer patients with the following goals:
- maintain blood pressure below 130/80
- maintain optimal blood sugar level
- aim for HbA1c of <=7%
- maintain and optimize lipid profile
- standard monitoring of diabetes
- lifestyle modifications with an emphasis on a balanced diet and exercise
- metformin and statins are optional treatments in these patients
- educating patients about signs and symptoms of cardiovascular disease
- identifying patients at risk to develop cardiovascular disease, including those with a history of ischemic heart disease, a history of cerebrovascular disease, congestive heart failure, peripheral arterial disease, hypertension, COPD, and renal impairment
- frequent monitoring of blood pressure levels, blood glucose, and lipid profile
- lifestyle modifications, which include a balanced diet and regular standardized exercise program. Patients should exercise for a minimum of 150 minutes per week with moderate intensity or 75 minutes per week of vigorous exercise.
- Smoking cessation and avoidance of alcohol are highly recommended
- consideration of aspirin 81 milligrams preventative therapy
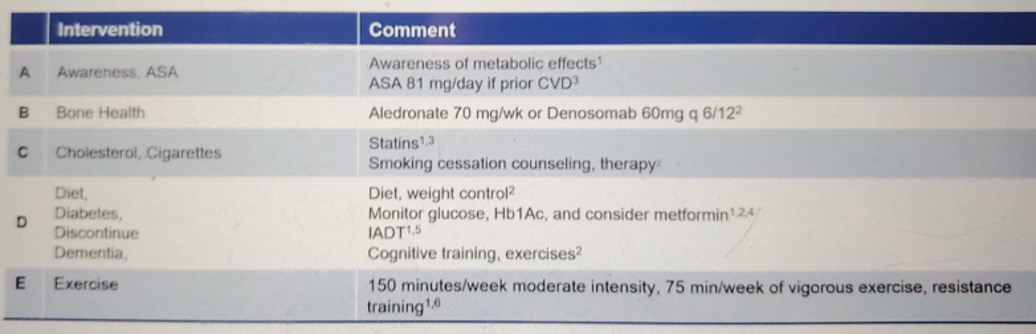
Dr. Klotz summarized his recommended ABCs of ADT management in Table 2.
Table 2 – ABCDE of ADT management:
In the next part of this talk, Dr. Klotz discussed the importance of monitoring serum testosterone levels in men receiving ADT. It is important to understand that testosterone fluctuation can occur during ADT use. The U.S. Federal Drug Administration (FDA) defines radical castration as testosterone levels below 50 ng/dl. The Bethesda consensus recommends a threshold for serum testosterone level after ADT to be 20 ng/dl. It is important to remember that with the use of LHRH receptor stimulation, there is an initial surge or flare that is associated with a rise in testosterone. Micro-surge or acute on chronic testosterone response reflects a transient testosterone increase that is also caused by LH receptor stimulation associated with subsequent agonist injections. Lastly, testosterone breakthrough is a rise in testosterone above a predetermined threshold, occurring anytime after the first month of treatment. Treatment failure refers to a prolonged breakthrough defined as over 2 testosterone measurements above the threshold. Due to these, testosterone suppression should be routinely monitored. Scheduled monitoring of testosterone and prostate-specific antigen throughout the treatment period is important so that we can ensure continuing treatment efficacy. Adequate testosterone suppression may play a role in castrate-resistant prostate cancer development. Currently, the National Comprehensive Cancer Network (NCCN), guidelines do not include testosterone levels as part of the screening or monitoring accommodations.
ADT remains the foundational treatment for prostate cancer. Approximately 40% of men receive ADT within six months of diagnosis of prostate cancer. Bilateral orchiectomy, the original form of ADT, is still used worldwide, more in the developing world. Medical ADT options are the gold standard where they are available. Intermittent androgen deprivation therapy is a cyclic therapy, with the cessation of ADT, allowing androgen recovery, and should be considered in the absence of extensive metastatic disease (Figure 2).
Figure 2 – Cyclic intermittent androgen deprivation therapy:
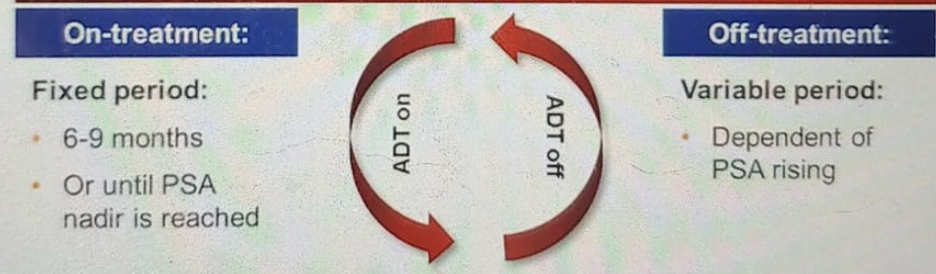
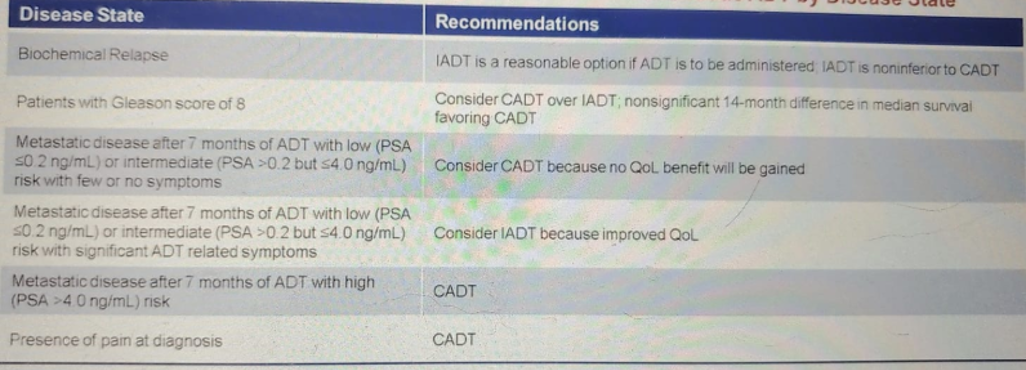
There are numerous advantages of intermittent ADT. It leads to improved quality of life, a prolonged period of androgen independence, reduces side effects associated with ADT, and decreases the cost of care. However, there is a modest risk of progression while on intermittent ADT compared with continuous ADT. If the prostate-specific antigen (PSA) levels rise rapidly, then continuous ADT should be started and maintained. Intermittent androgen deprivation therapy has been shown to be equivalent in cancer-specific survival and disease progression survival when compared to continuous ADT. In a meta-analysis assessing more than 3600 patients, the cancer-specific survival and disease progression were shown to be similar between intermittent and continuous ADT. No difference has been shown in overall survival as well between Intermittent and continuous ADT. At this point, Dr. Klotz showed a summary table, which aids in consideration of intermittent versus continuous androgen deprivation therapy (Table 3).
Table 3 – Factors to consider when choosing continuous and intermittent androgen deprivation therapy:
The last topic discussed in this encompassing talk was the role of ADT in the ARAT era. Almost all metastatic prostate cancer trials have demonstrated improved survival with the addition of a new androgen receptor antagonist or chemotherapy to ADT (Table 4).
Table 4 – Improved survival in metastatic prostate cancer trials with the addition of novel therapies to ADT:
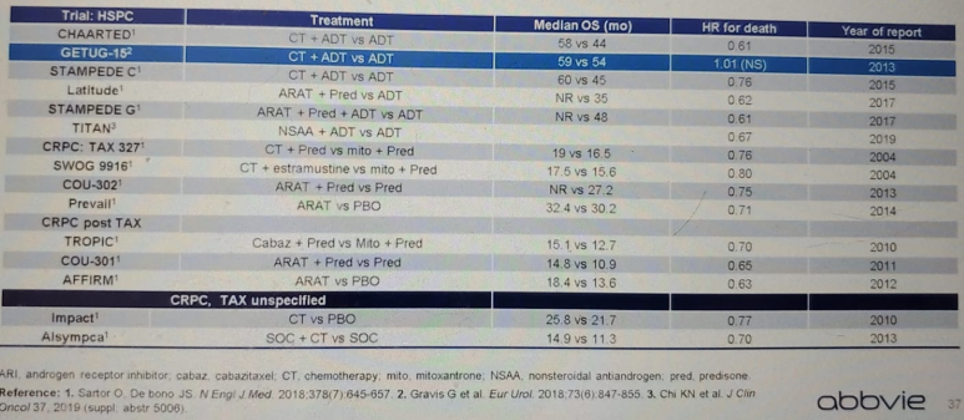
Chemotherapy + ADT has been shown to improve survival in metastatic hormone-sensitive prostate cancer, as was shown in the CHAARTED study, Androgen Ablation Therapy With or Without Chemotherapy in Treating Patients With Metastatic Prostate Cancer (CHAARTED). This trial demonstrated a 13.6 months longer overall survival with ADT and chemotherapy compared with ADT alone after a median follow-up of 28.9 months. Additionally, the STAMPEDE trial, Systemic Therapy in Advancing or Metastatic Prostate Cancer: Evaluation of Drug Efficacy (STAMPEDE), demonstrated that men receiving ADT in addition to chemotherapy and Prednisolone had a 22% and 39% improvement in median overall survival and failure-free survival, respectively, compared with the ADT alone group. Generally speaking, men receiving ADT plus chemotherapy demonstrate an improved absolute four-year survival rate.
In a very similar manner, in the LATITUDE trial, Abiraterone Acetate Plus Prednisone in Patients With Newly Diagnosed High-Risk Metastatic Castration-Sensitive Prostate Cancer (LATITUDE), a 38% and 44% reduction in the risk of death was shown in patients treated with abiraterone and ADT compared with the ADT alone group, at 30.4 months and 2 years. Moreover, the STAMPEDE trial demonstrated that ADT plus ARAT had a 37% reduction in the risk of death, compared to ADT alone.
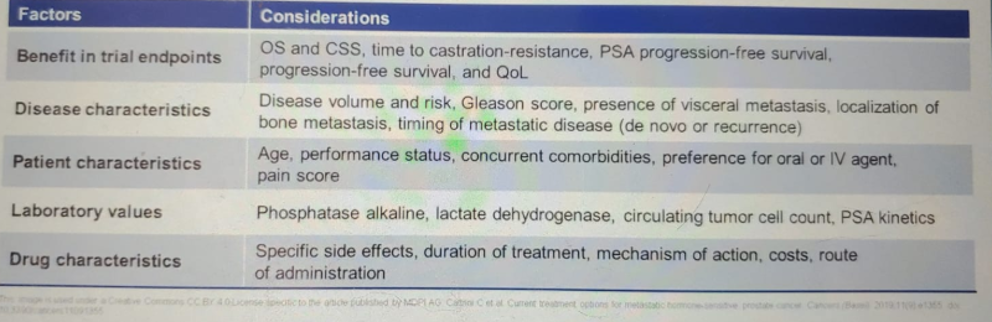
Dr. Klotz summarized some important potential decision-making factors in metastatic hormone-sensitive prostate cancer (Table 5).
Table 5 – Potential Decision-Making factors in metastatic hormone-sensitive prostate cancer:
Dr. Klotz concluded his talk with a summary and stated that the adverse effects of ADT often mimic testosterone deficiency and should be monitored. ADT is associated with an increased risk of unwanted adverse effects, which include metabolic syndrome, cardiovascular disease, liver disease, and many others. Testosterone and PSA should be routinely monitored to confirm that the treatment is working. Lower testosterone breakthrough rates improved time to castrate-resistant prostate cancer. Intermittent androgen deprivation therapy has shown comparable efficacy to continuous androgen deprivation therapy, with improved quality of life and reduction in the associated adverse effects. Lastly, there have been numerous clinical trials in the metastatic prostate cancer space, showing improved survival with the combination of ADT and either chemotherapy or ARAT.
Presented by: Laurence Klotz, MD, FRCSC, Professor, Department of Surgery, University of Toronto, Chief, Division of Urology, Sunnybrook Health Sciences Center, Chair, Canadian Uro-Oncology Group and NCIC GU Site Group, Editor in Chief (founding), Canadian Journal of Urology, Chair, Global GU Oncology Group
Written by: Hanan Goldberg, MD, MSc., Urology Department, SUNY Upstate Medical University, Syracuse, NY, USA, @GoldbergHanan at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020


Comments
Post a Comment