Cancer 'the best way to die'? You couldn't be more wrong if you tried ...
Do PSA Levels Help Stage Prostate Cancer?
Prostate-specific antigen (PSA) is a protein that forms in the prostate gland. A PSA test calculates PSA levels in the blood. While it cannot stage cancer by itself, it is a useful screening tool.
Prostate cancer is a common form of cancer that affects males. It is the most common cancer to receive a diagnosis in males worldwide. Prostate cancers may grow relatively slowly and can take up to 10 years for significant symptoms to develop.
Diagnosing prostate cancer early on enables a prompt treatment plan. This can increase the likelihood of successful treatment and reduce the chances of the cancer spreading and causing morbidity or mortality. PSA testing is the most common method of testing for prostate cancer, alongside transrectal ultrasound and prostate biopsies.
PSA testing is useful when working out the presence of cancer, how it is progressing, and whether PSA levels increase after treatment. However, PSA testing is relatively nonspecific, as a rise in PSA levels is not always due to a harmful tumor.
Read on to learn more about PSA levels and their role in monitoring prostate cancer.
PSA is a protein that can form in both regular cells, as well as malignant cancerous cells in the prostate gland. These proteins enter the bloodstream, which enables a medical professional to measure PSA levels from a blood sample.
PSA testing measures the concentration of PSA in the blood. This can help when assessing for prostate cancer, particularly when making an initial diagnosis.
PSA levels alone cannot indicate stages of prostate cancer. A doctor may use PSA levels as a screening tool for people at risk of developing prostate cancer. A doctor may also use PSA levels to monitor prostate cancer and whether the treatment is effective. After successful treatment, PSA levels can also indicate if cancer has recurred.
Additionally, PSA levels can vary due to a range of factors, so it is best to use other tests to support the results of a PSA analysis.
There are four main stages of prostate cancer. Classification depends on where the cancer spreads to and, therefore, how curable it is. If cancer cells spread from the prostate, they usually go to the bones or lymph nodes.
The stages of prostate cancer are as follows:
As stages of prostate cancer increase, a person's outlook worsens, and the cancer becomes more difficult to treat.
Read on to learn more about the stages of prostate cancer.
As well as having malignant prostate cancer cells, other factors can increase PSA levels in the blood. This reduces the reliability of PSA testing when assessing prostate cancer.
Reasons for high PSA levels can include:
On the other end of the scale, 5-alpha reductase inhibitors can reduce PSA levels by 50% over 6–12 months. A doctor may prescribe these medications to help treat BPH.
Read on to learn more about other causes of elevated PSA levels.
Although testing PSA levels is not always a specific method, it is currently the most common tool when assessing prostate cancer. Data show that mortality from prostate cancer has decreased by 44% since PSA testing became more accessible at the start of the 1990s.
Other types of prostate cancer tests include:
Read on to learn more about prostate exams.
Diagnosing prostate cancer is important for containing and treating the cancer. Prostate-specific antigen (PSA) testing is a common diagnostic tool that measures PSA levels in the blood.
PSA is a protein that comes from the prostate gland and can develop into cancer cells. Therefore, identifying a high concentration of PSA in the blood can indicate the presence of prostate cancer. However, other factors, such as harmless prostate enlargement, can also increase PSA levels. As such, while PSA testing cannot stage prostate cancer, it is an important screening and monitoring tool.
How A New 15-minute MRI 'scan In A Van' Could Spot Prostate Cancer Sooner
At the age of 58, Paul Rothwell decided to take up an invitation for a prostate cancer check.
He had no symptoms and had been warned that the standard prostate specific antigen (PSA) blood test was notoriously unreliable.
Nevertheless, he was delighted when his results came back with a reading of 1.5 (below the threshold of 3, the level that would require further investigation for his age).
However, Paul, a semi-retired TV producer from London, was also part of a research trial called ReImagine, which was looking at whether a new 15-minute MRI — the prostate equivalent of a mammogram for breast cancer — is better at diagnosing prostate cancer than the PSA test.
To his surprise, the results of his MRI scan carried out in April 2020 revealed that not only did he actually have the disease, but it was aggressive enough to need treatment.
At the age of 58, Paul Rothwell decided to take up an invitation for a prostate cancer check
'Without the MRI scan I would never have known,' says Paul, 62, who is married with two daughters.
Following the diagnosis, in March 2021, he underwent a treatment called focal therapy on the NHS.
The two main treatments for prostate cancer — surgery to remove the entire prostate or radiotherapy — can be highly effective, but carry the risk of potential side-effects, such as incontinence and impotence.
Focal therapy is more precise, treating the cancer itself rather than the whole prostate.
Paul had a form of focal therapy called high-intensity focused ultrasound (HIFU), which uses heat to target the cancer. He is now cancer free.
'Without the MRI scan, I could have gone for ten to 15 years without knowing I had prostate cancer, by which time it would probably have been more advanced and difficult to treat,' says Paul.
'I feel incredibly fortunate that I was able to have the scan.'
Now, a new trial is about to start inviting middle-aged men for the same screening as Paul had, but via a drop-in 'scan in a van'.
The vehicle will be parked next to West Ham United's football ground in the Olympic Park, London within weeks, with football fans and shoppers among those who could benefit.
The 'scan in a van' scheme is part of a trial of 800 men aged 50 to 75, the biggest ever using the 15-minute MRI.
Three hospitals as well as the van will be involved in the trial. It builds on two previous trials of the 15-minute MRI.
The first — the Prostagram study, carried out by Imperial College London — showed that the scan picks up twice as many high-risk prostate cancers compared to a PSA test followed by a biopsy.
In the second, the ReImagine trial, at University College London (UCL), the 15-minute MRI has been compared with a PSA blood test to see which is more effective at diagnosing cancer.
The results — due to be published shortly in the journal BMJ Oncology — are 'very promising', according to Caroline Moore, a professor of urology, who led this recent study.
However, ReImagine also revealed that men most likely to be affected by prostate cancer (such as those from black ethnic backgrounds) were less likely to come forward for tests.
The aim of the newest trial, called Limit, is two-fold: to see if the scan is more effective than the PSA at detecting risky cancers, and whether providing screening in the community can encourage more men from a wide variety of ethnic groups to come forward.
The 'scan in a van' scheme is part of a trial of 800 men aged 50 to 75, the biggest ever using the 15-minute MRI (file photo)
The results of the trial, should they be positive, will form part of the growing body of evidence that could tip the balance towards a national screening programme for prostate cancer.
Each year, 52,000 men in the UK are diagnosed with the disease. By the time around 16 per cent are diagnosed in England and Wales, the disease has spread, according to figures from the National Prostate Cancer Audit, and more than 12,000 men die each year.
As the Mail reported last week, there is an alarming postcode lottery in prostate cancer care that means men in the North-East are nearly six times more likely to be diagnosed late than men treated in London, for instance.
British scientists are working hard to address these inequalities. Improving diagnostic tests and making these tests more accessible, by introducing mobile testing units, are among the solutions being investigated.
'We know from trial results that the 15-minute MRI is a good way to detect risky cancers that are more likely to cause problems,' explains Professor Moore.
Prostate cancer screening studies have found that some men are reluctant to come forward for tests, especially those at greatest risk, she adds.
Men from black ethnic groups have twice the risk of prostate cancer, for example [scientists don't know why but it might be linked to genes], 'but are not always reached by the traditional screening approaches such as an invitation letter through their GP,' she told Good Health.
'The Limit trial will be open to men of all backgrounds. However, we hope, by offering tests for prostate cancer in the community, with the van and without the need for an appointment, we will be able to reach a wider group.'
'Without the MRI scan, I could have gone for ten to 15 years without knowing I had prostate cancer, by which time it would probably have been more advanced and difficult to treat,' says Paul
This is not the first time that a 'man van' has been used to encourage men to come forward for health checks.
Last year, a mobile clinic was launched in London to encourage men over 45, who are from groups less likely to receive regular health checks, to come forward.
Results from the pilot study showed — during visits to seven locations in South London, including construction sites — that more than 600 men visited the mobile clinic for checks, including a PSA test: 14 were diagnosed with prostate cancer, 18 with diabetes, a quarter with possible high blood pressure and nearly three quarters with obesity.
Currently, a PSA test remains the most common way of seeing who needs further testing, despite the test being unreliable: 75 per cent of men who get a high score are actually cancer-free (a false positive), while 15 per cent who do have cancer don't have a raised PSA level (a false negative).
This leads to men without cancer going through unnecessary tests, and men with cancer being diagnosed late.
All men over 50 can ask their GP for a PSA test if they're concerned about prostate cancer — they don't need to have any symptoms.
A PSA score of 3 or above (if the man is aged over 50; over 4 if he's 70) requires further investigation.
However, PSA levels can rise as a result of other factors, such as after vigorous cycling or sex.
The new Limit study will be carried out in three hospitals — Addenbrooke's in Cambridge, University College London Hospital and The Christie in Manchester — as well as via the mobile screening van.
Men having the tests in hospital will be invited through their GP, but those attending the mobile screening unit can 'drop in'.
At each of the four sites, 200 men in total will be given both the PSA test and a 15-minute MRI — a process that will take around an hour (including the paperwork), says Professor Moore.
The MRI scan is a 'trousers on' test. Those tested in the van will receive their results on the spot from a trained urologist, who will help them determine the next steps, if needed, while those tested in hospital will get theirs two weeks later.
Researchers at UCL will monitor the results and who takes up the offer of screening. To participate in the trial, which is expected to take three years, men must be aged 50 to 75, with no symptoms or a previous diagnosis of prostate cancer.
Men with a hip replacement aren't eligible as the artificial joint makes the images difficult to read.
Gamal Turawa, 60, from Bedfordshire, was aware of his increased risk of prostate cancer, as he comes from a black ethnic background, so he joined the Prostagram trial in 2018.
Gamal Turawa, 60, from Bedfordshire, was aware of his increased risk of prostate cancer, as he comes from a black ethnic background, so he joined the Prostagram trial in 2018
'I saw a Facebook post about the trial and decided to take part,' says Gamal, a motivational speaker and former police officer.
'I had no symptoms and there is no family history of the disease, but I have always been aware of the risk and was curious given my age and background.'
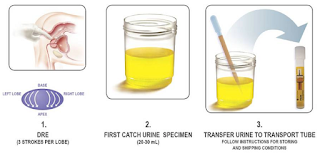
He underwent a PSA blood test, a rectal examination and the 15-minute MRI scan at Hammersmith Hospital in London.
'Of the three tests, I preferred the MRI, because it was less invasive,' he told Good Health.
After a couple of weeks, Gamal received the results, giving him the all clear.
'Having the MRI gave me much greater confidence in the result,' he says. 'It should be made available for all men — and I support a prostate screening programme.'
What Is Aggressive Prostate Cancer?
While most prostate cancers grow slowly, some may classify as aggressive prostate cancers based on stage and grade.
Prostate cancers mostly consist of adenocarcinomas, which develop within the prostate gland cells.
In general, cancers that are "aggressive" are those that can form, grow, or spread rapidly. In some cases, having aggressive cancer can mean that the disease is more severe or has come back after treatment.
Anaplastic prostate cancer is an aggressive cancer that involves the nervous and endocrine (neuroendocrine) systems. It's not considered common.
Aggressive prostate cancer requires careful diagnosis and prompt treatment.
Aggressive prostate cancer has a different cellular makeup than adenocarcinomas of the prostate gland, which can cause it to grow and replicate quickly. It also sometimes resists certain hormone treatments typically used for prostate cancer.
A doctor may also diagnose prostate cancer as "aggressive" based on data collected from the following:
Gleason scoresBased on a biopsy sample, having a Gleason score of 8–10 could indicate a risk of cancer spreading from the prostate to other parts of the body.
Prostate-specific antigen (PSA) blood testsA score of 20 or above could indicate high risk prostate cancer. However, in hormone-resistant aggressive subtypes, PSA may be at a low level in the initial stages.
TNM cancer staging systemThis staging system assesses the size of the tumor and whether the cancer has spread to any lymph nodes or more distant areas in the body. Category T4, N1, or M1 indicates a large tumor with lymph node spread (metastasis), and is often associated with aggressive prostate cancer.
The TNM staging system is also responsible for the common number staging system, which ranges from 0–4, with stage 3 indicating aggressive cancer and stage 4 meaning cancer has spread to distant organs.
Cancer gradingGrade 3 indicates that the cancer cells are abnormal and are more likely to grow aggressively.
Aggressive prostate cancers spread rapidly. When diagnosed at an advanced stage, the cancer classifies as stage 3. This stage means that the cancer may have spread outside of the prostate gland.
The diagnosis of aggressive prostate cancer may also occur at stage 4. Stage 4, or metastatic cancer, is the most advanced stage and means that cancer has spread to at least one other organ of the body.
Prostate cancer — including aggressive subtypes — may or may not have symptoms until the tumor has become large.
As the cancer becomes more aggressive or advanced, you might experience:
While the exact cause of aggressive prostate cancer isn't known, this subtype may develop as a result of hormone treatment resistance. This may explain why aggressive prostate cancers may be more common in those who have previously undergone treatment for adenocarcinoma.
Researchers are also exploring the possibility of genetic mutations that could play a role.
There's no single timeline, but aggressive prostate cancer progresses in the body rapidly. This tendency is in stark contrast to traditional adenocarcinomas of the prostate gland, which tend to progress very slowly for years.
Aggressive prostate cancer tends to present with metastasis in the bones and lymph nodes in the pelvic region despite a low PSA level.
A doctor may confirm aggressive prostate cancer with the following tests:
Due to a high rate of spread and possible resistance to hormone-based treatments, aggressive prostate cancer isn't considered curable.
The goal is to undergo treatments that may help shrink the tumor, prevent further spread, and help reduce prostate cancer symptoms.
Treatment options may help manage the spread of aggressive prostate cancer while preventing the advancement of the cancer and improving symptoms.
Surgery may be the most effective treatment strategy for aggressive prostate cancers that have not yet spread to distant areas of the body. Surgery may involve removing tissues from the prostate or removing the prostate gland.
Additional treatments for aggressive prostate cancer include:
While most cases of prostate cancer are slow-growing, aggressive forms may have even lower life expectancy if they are not detected and treated early.
According to data between 2013 and 2019 from the National Cancer Institute's Surveillance, Epidemiology, and End Results Program (SEER), the 5-year survival rate for all cases of prostate cancer was 97.1%, and for prostate cancers that spread to distant areas beyond the original tumor site was 34.1%
The exact outlook for aggressive prostate cancer depends on numerous factors. According to a 2020 clinical review of 94 cases of aggressive prostate cancer, the average life expectancy was less than 24 months.
Aggressive prostate cancer is a subtype that grows quickly and may possibly be resistant to hormone therapies. While it is not considered curable, treatments are available to help prevent the cancer from spreading further and improve the quality of life.



Comments
Post a Comment